Abstract
Paracetamol is frequently used as an analgesic and antipyretic across the world. However, there is no data on Indian patients regarding the safety and efficacy of paracetamol + lignocaine injection in patients with high-grade fever. Hence, a prospective analysis was conducted to assess the safety and efficacy of paracetamol and lignocaine injection in patients with high-grade fever and mild-to-moderate body pain. The study is a real-world prospective study. The results showed that following intervention with paracetamol and lignocaine injection, 98% patients showed resolution of fever and 58% patients showed improvement in pain symptoms. The authors suggest that clinicians should consider paracetamol and lignocaine injection in patients with high-grade fever and associated pain and discomfort.
Keywords: Paracetamol, paracetamol + lignocaine injection, high-grade fever
The febrile response is a complicated event involving several immunologic and physiologic pathways. It is the most frequently observed physical sign in critically ill patients related to systematic inflammatory response syndrome or infections.1 Antipyretics are commonly employed in patients with fever. Among the antipyretics, paracetamol is one of the most commonly used synthetic, nonopioid and centrally acting drug. It acts by inhibiting the cyclooxygenase-3 and the prostaglandin synthesis, within the central nervous system, leading to resetting of the hypothalamic heat-regulation center.2
Paracetamol is used to lower temperature in patients with fever as untreated fever places additional physiological stress on patients who are already ill.3 While paracetamol is approved for the treatment of pain and fever in several countries worldwide, there is not enough real-world data on Indian patients regarding the effect of intravenous (IV) paracetamol given in combination with lignocaine in patients with high-grade fever. Such data would help clinicians in making informed decisions about the use of paracetamol-lignocaine combination in their patients. Hence, a prospective study was conducted among patients suffering from high-grade fever and mild-to-moderate body pain to assess and establish the safety and efficacy of IV paracetamol + lignocaine combination in high-grade fever patients.
METHODS
The study is a real-world prospective study to assess the efficacy of IV paracetamol + lignocaine combination and the occurrence of adverse events in patients with high-grade fever and pain. All patients with high-grade fever (>102°F) and mild-to-moderate body pain, aged 18 years or above, and those willing to give feedback were included in the study. Any patient with other serious ailments such as acquired immunodeficiency syndrome (AIDS), cancer, renal or hepatic dysfunction were excluded from the study. After the patients were enrolled for the study, preliminary body temperature reading was taken, and associated symptoms, if any, were also noted. Patients were administered paracetamol + lignocaine IV or IM and patient feedback of pain score on a visual analog scale (VAS) were recorded after administration. The temperature reading was taken after 15 to 30 minutes of administration and any change in associated symptoms was also captured. The patients were checked for the appearance of any side effects such as skin rashes, nausea, vomiting, etc.
Written consent was taken formally from the study participants after informing them about the study, use of the medicine in their condition, and any related side effects that may occur. The data was collected anonymously. Analysis of the responses was carried out by calculation of simple percentages.
RESULTS
The study included 109 patients (31 females and 78 males). All patients had baseline fever (>102°F) and 101 patients reported pain as one of the associated symptoms. Thirteen patients were diagnosed with dengue, while there were 1 patient each with diabetes, urinary tract infection, compound fracture and lower rib pain.
Within 30 minutes of using parenteral paracetamol + lignocaine, only 2 patients reported low-grade fever, while 42 patients (38.5%) reported low-grade pain (based on VAS score). Figure 1 depicts the baseline and post-intervention data of the patients.
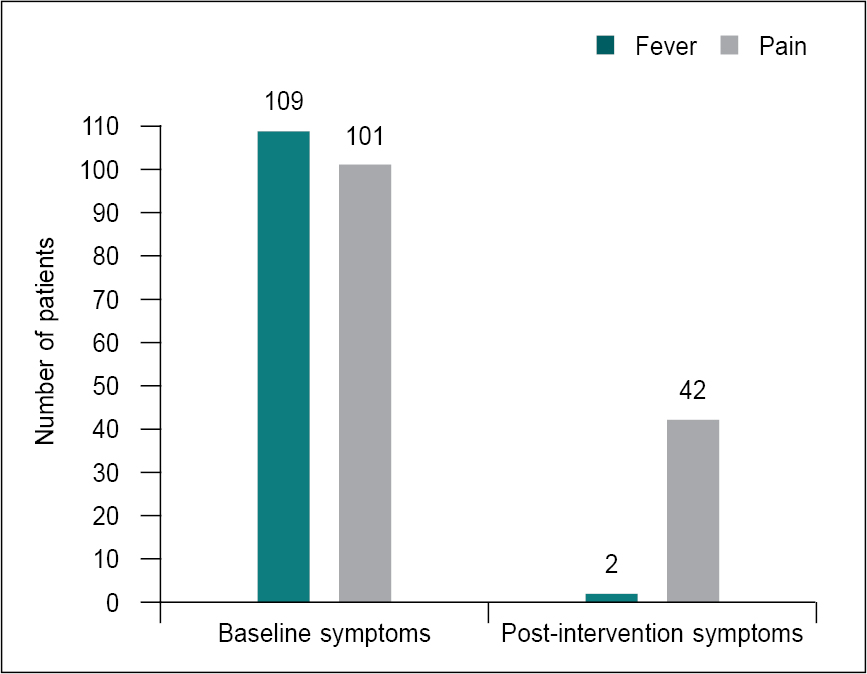
Figure 1. Baseline and post-intervention symptoms in the study participants.
None of the patients reported any adverse effects following the use of parenteral paracetamol + lignocaine. Figure 2 shows the patient responses in terms of efficacy of paracetamol + lignocaine combination on fever and pain before and after the treatment.
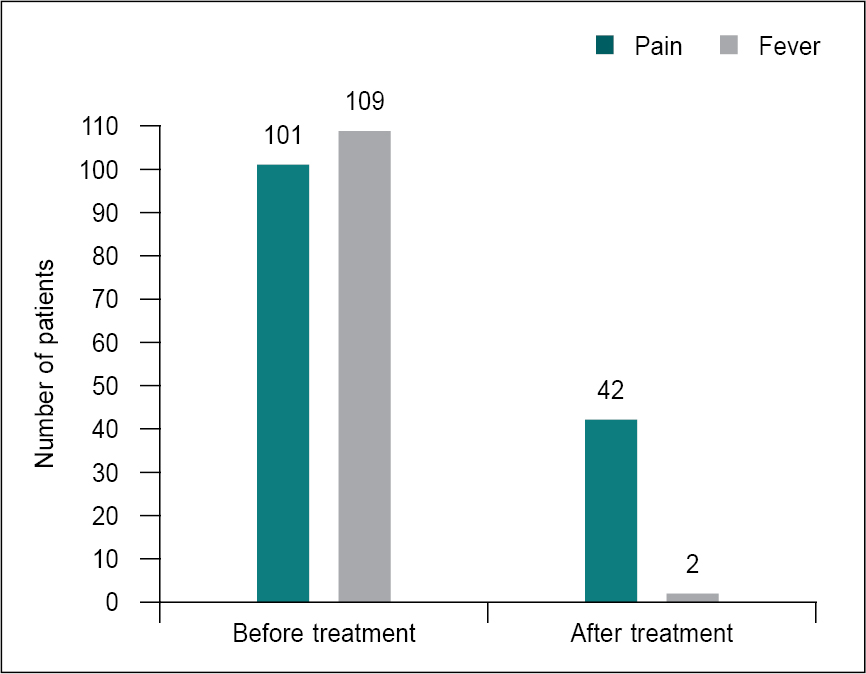
Figure 2. Patient response after paracetamol + lignocaine injection (58% patients showed relief in pain, while 98% patients showed resolution of fever).
DISCUSSION
Paracetamol is recommended for use around the world as the most popular agent for the treatment of mild-to-moderate pain due to its analgesic and antipyretic activity.4
Injectable paracetamol was approved in 2002; its onset of action is within 5 to 10 minutes of administration, peak effect occurs in 1 hour and the duration of action lasts for 6 hours. It does not have any major adverse effects, has no sedative effect and does not interfere with platelet or kidney functions.5
A double-blind placebo-controlled randomized trial showed that parenteral paracetamol-lignocaine combination led to significantly higher and longer analgesic effects compared with the same dosage of plain paracetamol administered in oral form.6 Patients’ response to pain as per VAS score was found to be 0 in the majority of cases, while a few reported grade 1 and 2 pain (6.9% and 23.7%, respectively).
Our study also showed that paracetamol + lignocaine injection led to a significant reduction in fever within 15 to 30 minutes of administration, which lasted for at least 6 hours. None of the patients reported any side effects. These results are in sync with an earlier study where Jarde and Boccard had demonstrated that parenteral paracetamol has a quicker onset of action (at 15- and 30-minutes post-dose) and was also more efficacious with significantly fewer patients who required remedication.6 In the present study, the paracetamol + lignocaine injection also showed a longer duration of action.
It has also been shown in an earlier study that the combination of paracetamol and a local anesthetic also reduce the pain caused by injections.7
CONCLUSION
The clinical implication of our study is that the onset of action of paracetamol in combination with lignocaine administered intravenously, can occur within 15 to 30 minutes. There are no adverse effects, there is an effective reduction of associated signs and the duration of action is much longer. Paracetamol + lignocaine injection can be effective when given to patients with high-grade fever and leads to an effective reduction in VAS pain score. Due to the combination of paracetamol and lignocaine, there is no pain at the site of injection; hence, it can be easily administered to the patient. The results of this study establish that short-term treatment of moderate pain and fever with paracetamol + lignocaine given via IV route is clinically justified. Physicians should consider using IV paracetamol in combination with lignocaine in patients with fever and associated discomfort or pain to relieve patient suffering and reduce pain, which may help provide optimal patient care.
REFERENCES
- Honarmand H, Abdollahi M, Ahmadi A, Javadi MR, Khoshayand MR, Tabeefar H, et al. Randomized trial of the effect of intravenous paracetamol on inflammatory biomarkers and outcome in febrile critically ill adults. Daru. 2012;20(1):12.
- Chiumello D, Gotti M, Vergani G. Paracetamol in fever in critically ill patients - an update. J Crit Care. 2017;38:245-52.
- Young P, Saxena M, Bellomo R, Freebairn R, Hammond N, van Haren F, et al; HEAT Investigators; Australian and New Zealand Intensive Care Society Clinical Trials Group. Acetaminophen for fever in critically ill patients with suspected infection. N Engl J Med. 2015;373(23):2215-24.
- Vaghela KR, Dave UM, Jadeja CA, Chaudhari DR, Gohil JJ. A comparative study of intravenous febrinil vial (150mg/ml) vs intravenous paracetamol (1gm/100 ml) pint formulation for postoperative analgesia. Indian J Clin Anaesth. 2020;7(1):83-7.
- Duggan ST, Scott LJ. Intravenous paracetamol (acetaminophen). Drugs. 2009;69(1):101-13.
- Jarde O, Boccard E. Parenteral versus oral route increases paracetamol efficacy. Clin Drug Investig. 1997;14(6):474-81.
- Hayat M, Afshan G, Nasir M, Asghar S, Monem A. Efficacy of intravenous paracetamol in combination with lidocaine pretreatment for reducing pain during injection of propofol. Cureus. 2020;12(2):e6926.