Abstract
Introduction: Now-a-days, young people below age of 40 years without known risk factors are presenting with stroke. The cause of stroke should be found so that recurrence and other complications can be prevented. Case description: An 18-year-old female presented with holocranial headache, focal seizures with impaired awareness and left hemiparesis. The upper limb pulses were absent on both sides, while pulses in lower limbs were present. MRI scan of brain revealed infarct in right middle cerebral artery territory. CT angiography brain showed luminal narrowing in upper limb arteries, carotid artery and vertebral artery. She was treated with antiplatelet drug, tablet carbamazepine, tablet methotrexate with folinic acid and she improved. Discussion: Takayasu arteritis is an inflammatory vasculitis disease causing stenosis in medium and large sized arteries. It can present as stroke, myocardial infarction, aortic insufficiency, retinal ischemia, renal failure and hypertension. Conclusion: Takayasu arteritis is one of the rare causes of stroke, which when detected should be promptly treated to prevent further episodes of stroke and other system complications.
Keywords: Stroke, Takayasu arteritis, vasculitis
Takayasu arteritis is a large vessel vasculitis, which mostly affects the aorta, carotid arteries and renal vessels. Takayasu arteritis usually presents with fever, myalgia, night sweats, arthralgia and absence of peripheral pulses. Despite luminal narrowing of large vessels, it rarely presents with stroke as an initial presentation. Patients commonly present with limb claudication, coronary artery disease and renal hypertension.
METHODS
Detailed history and clinical examination of the patient was done. Blood investigations, i.e., complete blood count, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), renal function test, ANA (antinuclear antibody) profile was done. Radiological investigations, i.e., ultrasound of neck, arterial Doppler of upper limbs and lower limbs, computed tomography (CT) angiogram of brain, chest and abdomen and magnetic resonance imaging (MRI) of brain was done. Case was discussed with Rheumatologist regarding disease-modifying medications to prevent future relapse. Informed consent was taken from the patient.
CASE DESCRIPTION
An 18-year-old female presented with holocranial, dull aching headache aggravating on coughing and bending forward for 2 days. On the third day of her illness, she had 1 episode of focal seizures involving left upper and lower limb, up rolling of eyes, followed by post-ictal confusion lasting for 3 minutes. It was followed by weakness of left upper and lower limb. There were no associated previous comorbidities. There was no similar history in the family members.
On general examination, pulses were absent in both the radial and brachial arteries; both carotid pulses were weak. She had left upper motor neuron type of facial palsy, left hemiparesis with power 3/5, deep tendon reflexes 2+ in all 4 limbs, with plantar-extensor on left side with circumduction gait. Her sensory, cerebellar, autonomic systems were normal.
Her blood work-up showed hemoglobin - 9.6 g/dL, total leukocyte count (TLC) - 10,200/cumm, TPC - 3,92,000/cumm, normal renal function test, ANA profile - negative, HIV test - negative, ESR - 100 mm/hr, CRP - negative, ultrasound neck - steno-occlusive disease in bilateral carotids.
MRI of brain showed acute infarct in right frontal lobe, right caudate nucleus, lentiform nucleus and right corona radiata (Fig. 1). Magnetic resonance angiogram (MRA) of intracranial vessels showed nonvisualization of intracranial part of right internal carotid artery and complete reformation of right anterior cerebral artery (Fig. 2).
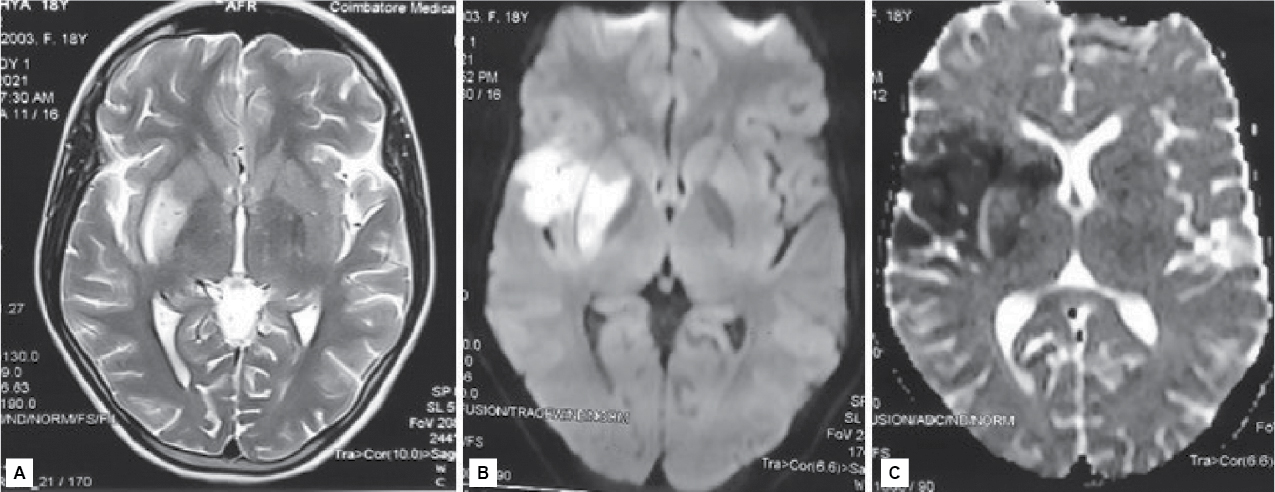
Figure 1. MRI of brain – A) T2/FLAIR; B) Diffusion-weighted imaging showing hyperintensity in right insular cortex and right lentiform nucleus; C) Attenuated diffusion coefficient showing hypodensity in the right gangliocapsular area, right insular cortex and caudate.

Figure 2. Magnetic resonance angiogram – right middle cerebral artery not visualized.
Arterial Doppler of upper limbs showed significant stenosis in the proximal subclavian artery. CT angiogram of brain (Fig. 3) and chest (Fig. 4) showed complete occlusion of right common carotid artery and 50% occlusion of left common carotid, 20% to 30% luminal narrowing of both internal and external carotid artery, occlusion of left and right vertebral artery, both subclavian artery occlusion (30% occlusion), both axillary, brachial, radial, ulnar artery and descending thoracic aorta (20% occlusion). Renal arteries, abdominal aorta, external and internal iliac arteries on both sides were normal.
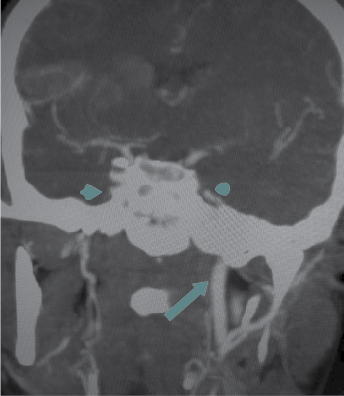
Figure 3. CT angiography of brain – Nonvisualization of infraclinoid part of right internal carotid artery, nonvisualization of right common carotid artery.
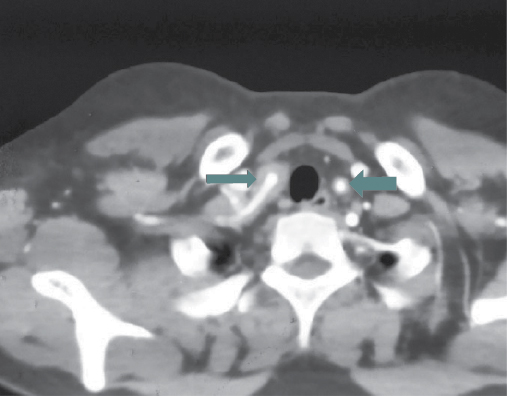
Figure 4. CT angiogram of chest blood vessels – mural thickening seen in both the subclavian arteries.
She met 3 out of 6 American College of Rheumatology (ACR) criteria. She had type IIB Takayasu arteritis.
She was treated with injection dexamethasone 8 mg BD, injection levetiracetam 500 mg BD and tablet aspirin 150 mg OD. Tablet methotrexate 7.5 mg once a week was started as advised by the Rheumatologist. Her power improved with minimal deficit. She was discharged with tablet methotrexate 7.5 mg once a week, tablet prednisone 20 mg, tablet aspirin 150 mg BD and tablet levetiracetam 500 mg BD, tablet folic acid 5 mg OD. On follow-up, she is doing well with no further episodes.
DISCUSSION
Takayasu arteritis is a large-vessel vasculitis of unknown cause affecting females aged 11 to 30 years. It affects aorta, carotid artery, renal and pulmonary artery and causes formation of thrombus leading to stenosis and obstruction of the blood vessels. The complications of Takayasu arteritis are vascular claudication, renal hypertension, congestive cardiac failure and coronary artery disease. Stroke occurs in 10% to 20% of cases having Takayasu arteritis. Possible cause of stroke in Takayasu arteritis include embolism from stenotic or occlusive lesions in the aortic arch and its main branches.1-3
For diagnosing Takayasu arteritis as the cause of the stroke, 1990 ACR criteria was used, according to which the patient should have at least 3 out of 6 criteria:
- Onset at age of 40 years or younger
- Claudication of an extremity
- Decreased brachial artery pulse
- Difference higher than 10 mmHg in systolic blood pressure between arms
- Presence of a bruit over the subclavian arteries or the aorta
- Arteriographic evidence of narrowing or occlusion of the entire aorta, its primary branches or large arteries in the proximal upper or lower extremities.2
The patient had type IIB Takayasu arteritis, which was concluded from the following 6 types based on angiographic involvement:
- Type I – Branches of the aortic arch
- Type IIa – Ascending aorta, aortic arch and its branches
- Type IIb – Type IIa region plus thoracic descending aorta
- Type III – Thoracic descending aorta, abdominal aorta, renal arteries or a combination
- Type IV – Abdominal aorta, renal arteries or both
- Type V – Entire aorta and its branches.4
The inflammatory process of vasculitis in Takayasu arteritis is mediated by T cells, macrophages and dendritic cells in the arterial wall. The inflammation starts in tunica media and adventitia followed by panarteritis. The aortitis leads to extensive fibrosis and increased wall thickness.1,2,5
On clinical examination, patients have loss or inequality of pulses in the upper limbs (known as Pulseless disease), asymmetric blood pressures between upper limbs or bruits heard in neck, supraclavicular region.1,2
Ultrasound Doppler of arteries, CT of brain, CT angiography and MRI of brain are the radiological modalities that help in diagnosing Takayasu arteritis and tell us about the affected vessels. Steroids are the first-line treatment. For long-term treatment, steroid-sparing drugs are used, i.e., methotrexate, cyclophosphamide, azathioprine. The patient should be started on immunomodulatory drugs to prevent the progression of the disease and to reduce the further involvement of the other unaffected blood vessels.6
Prognosis and recovery are good, with stable course of the disease on immunosuppressive therapy.6-8
CONCLUSION
Complete clinical examination and prompt evaluation of the cause of stroke in young patients can help in reducing morbidity and early rehabilitation to led a better quality of life. Proper guidance about Takayasu arteritis and continuation of immunomodulatory therapy can help these patients in avoiding future complications.
REFERENCES
- YuWen C, Chang CJ, Hsieh CT. Stroke as an initial presentation of Takayasu’s arteritis. Neurology Asia. 2015;20(2):177-80.
- Duarte MM, Geraldes R, Sousa R, Alarcão J, Costa J. Stroke and transient ischemic attack in Takayasu’s arteritis: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2016;25(4):781-91.
- Del Brutto OH, Lara-Terán J, Sánchez J, Lara-Montiel J. Cerebrovascular complications of Takayasu’s disease. Rev Neurol. 1996;24(131):803-5.
- Zhu FP, Luo S, Wang ZJ, Jin ZY, Zhang LJ, Lu GM. Takayasu arteritis: imaging spectrum at multidetector CT angiography. Br J Radiol. 2012;85(1020):e1282-92.
- Silver M. Takayasu’s arteritis - An unusual cause of stroke in a young patient. West J Emerg Med. 2012;13(6):484-7.
- Adams HP Jr. Takayasu disease and stroke. Practical Neurology. 2020 Jan;58-61.
- Schurch MA, Gerster JC. Takayasu’s arteritis-case report and review of the literature. Rev Med Suisse Romande. 2000;120(10):777-80.
- Hwang J, Kim SJ, Bang OY, Chung CS, Lee KH, Kim DK, et al. Ischemic stroke in Takayasu’s arteritis: lesion patterns and possible mechanisms. J Clin Neurol. 2012;8(2):109-15.