Abstract
Health care in India is undergoing a rapid change from its historical focus on acute disease management to a focus more on chronic and continuous care-based model for noncommunicable disorders. Health technology could be a game changer as it has a potential to optimize costs and effectively manage such operations. IT solutions are likely to become an integral part of process management, patient care and the hospital management information system in future. This brief communication describes the key enablers and limitations of using health technology in chronic diseases in developing countries like India.
Keywords: Health care, IT solutions, game changer, continuous care-based model, digital health, smart technology
Technology is now embedded in many facets of daily life for large numbers of people across the world, and despite the fact that populations as a whole are increasingly tech-literate, the health sector has been hesitant in its approach to new technologies and inefficient in implementation of those with a strong evidence base. Health technologies can be powerful tools in supporting, expanding and enhancing all domains of health, including but not limited to: health care services, health surveillance, health education, research, prevention and patient treatment and management.1
In addition, the convergence of health care with upcoming technologies like cloud computing and wireless technologies will improve accessibility and meeting the challenge of skilled manpower shortage.2 Several projects in India and other developing countries are already underway to assimilate health technology with existing health infrastructure.3
A recent study in rural India has shown that use of technology in the form of a mobile phone-based, nurse-facilitated clinical decision support system in primary care could improve the blood pressure and blood glucose control and has large potential to scale-up in resource-poor settings.
eHealth is defined by the World Health Organization (WHO) as use of information and communication technologies (ICT) for health, and includes the field of mHealth, which relates specifically to the medical or public health practices that are supported by mobile phones and other wireless devices. When member states of the WHO committed to work towards universal health coverage (UHC) in 2005, eHealth was made a priority in recognition of its “pivotal role” in achieving this aim and indeed WHO’s Report on the third global survey on eHealth, published in 2016, asserts that “It has become increasingly clear that UHC cannot be achieved without the support of eHealth.”4
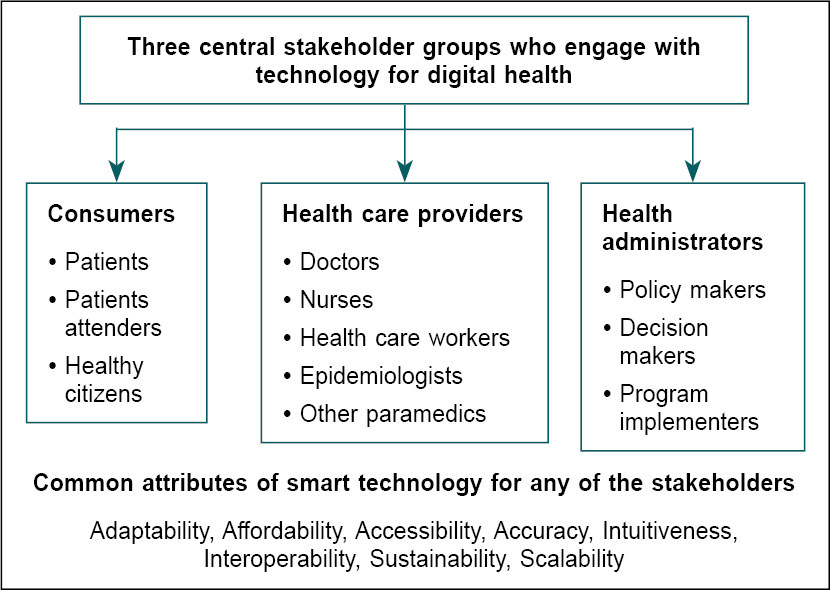
ENABLERS AND KEY STAKE HOLDERS OF HEALTH TECHNOLOGY
The key attributes for developing a sustainable and scalable model for health technology include to first define the problem with careful consideration of appropriate future integration into relevant health policies (Fig. 1). This should be followed by an appropriate identification of the technology users and the setting in which it has to be applied. And last but not the least, to use a highly iterative technology design and development process that incorporates the perspective of the user and also addresses scalability right from its inception.5 There are diverse benefits of utilizing health technology in the evaluation and management of chronic conditions. However, there are challenges that need to be addressed to ensure widespread and maximal utilization of technologies in health care delivery. A major concern raised by experts on these programs is ensuring availability of high-quality care to most individuals utilizing these support systems. In addition, the high cost that may be incurred in the development and dissemination of these technologies provides a challenge to health care institutions. More so in developing countries like India concerns regarding health literacy and poor electricity supply in remote areas were also raised in the forum.6 Also, given the vast cultural and ethnic differences within the same country, it is important to tailor the use of technology to specific populations and settings.
Figure 1. The key attributes for developing a successful program for health technology Obstacles for use of health technology in India.
 </p
</p
CONCLUSION
The use of digital technologies to support the achievement of health objectives has been a ‘hot topic’ in public health for well over a decade. In that period, there have been rapid advances in computing and mobile technologies, matched by ever increasing access to these technologies and expansion of wireless and mobile networks. Although issues of equity cannot be ignored in cases where interventions require access to personal devices, other technologies have the potential to improve the equitable provision of health services to individuals and communities who are otherwise outside the existing health care services.
REFERENCES
- Spangler J, Huth T, Xie R. Patient perspectives: an integral part of health technology assessment methodology. Int J Technol Assess Health Care. 2022;38(1):e85.
- Laktabai J, Platt A, Menya D, Turner EL, Aswa D, Kinoti S, et al. A mobile health technology platform for quality assurance and quality improvement of malaria diagnosis by community health workers. PLoS One. 2018;13(2):e0191968.
- Rai D, Bhattacharjee S, Dhakal R, Chattopadhyay K, Neupane D. Effects of mobile technology-based interventions in promoting mental health and psychosocial wellbeing among young people in low- and middle-income countries: a systematic review protocol. JBI Evid Synth. 2022 Oct 17. [Epub ahead of print]
- e-Health Code of Ethics (May 24). e-Health Ethics Initiative. J Med Internet Res. 2000;2(2):E9.
- Dingler T, Kwasnicka D, Wei J, Gong E, Oldenburg B. The use and promise of conversational agents in digital health. Yearb Med Inform. 2021;30(1):191-9.
- Lim LL, Lau ESH, Ozaki R, Chung H, Fu AWC, Chan W, et al. Association of technologically assisted integrated care with clinical outcomes in type 2 diabetes in Hong Kong using the prospective JADE Program: a retrospective cohort analysis. PLoS Med. 2020;17(10):e1003367.