Abstract
The case describes the anatomy and pathophysiology of the palatine tonsils and the development of intratonsillar abscess. The abscess can be caused by a suppurative focus that arises in acute tonsillitis when outward drainage is prevented, leading to pus accumulation in the tonsillar tissue. Dehydration or a history of peritonsillar abscess can also lead to intratonsillar abscess. The condition can be mistaken for tonsillolith or malignancy, such as lymphoma. A computed tomography (CT) scan is recommended for diagnosis, showing a low-density and ring enhancement. Aspiration using a large bore needle is the preferred mode of treatment, but if repeated aspirations fail, tonsillectomy may be necessary. Intratonsillar abscess is rare and so far only 29 cases have been reported.1 The differential diagnoses include lymphoma, which usually presents as unilateral enlargement of the tonsil, tonsillolith due to its appearance and peritonsillar abscess again due to the unilateral enlargement of the tonsil. This case is different as compared to other reported cases we did not do a CT scan as recommended by most of the studies (cost being a concern). Also, in this case, we resorted to surgery as the main modality unlike other cases wherein the surgeons opted to do an aspiration of the pus mainly keeping the intraoperative complications in mind.
Keywords: Intratonsillar abscess, chronic tonsillitis, quinsy, aspiration, tonsillectomy
Intratonsillar abscess is a condition which is rarely seen in the practice of an ENT surgeon. It is also diagnosed less often. It is formed in the parenchyma of the tonsil. Clinically, intratonsillar abscess may mimic chronic tonsillitis or quinsy (peritonsillar abscess). Tonsillitis, which usually affects children and rarely young adults, is a commonly seen entity in ENT outpatient departments (OPDs). Treatment options include antibiotics, incision and drainage and tonsillectomy.
CASE REPORT
A 32-year-old male presented to the ENT OPD with enlargement of the left tonsil since 3 to 4 years with off and on increase in the size of the swelling coinciding with bouts of upper respiratory infections (URI) (Fig. 1). During the URI episodes, the patient also complained of odynophagia, halitosis and a raw sensation in the throat and fever. He relied on home remedies to get relief from these symptoms.

Figure 1. Patient’s intraoral picture showing enlarged tonsil on the left side with a prominent yellowish growth on upper pole of tonsil.
After examination, he was prescribed capsule amoxicillin 500 mg 1-0-1, diclofenac sodium 1-0-1, tablet paracetamol 1-0-1, tablet ranitidine 1-0-1 on an empty stomach and a povidone-iodine based mouth gargles for a week so that the acute bout subsided.
Follow-up examination after 10 days revealed that the left tonsil including the yellowish growth on the upper pole of the same tonsil had not regressed in size.
He was advised to undergo bilateral tonsillectomy keeping lymphoma as a probable diagnosis in mind.
Prior to tonsillectomy his blood and urine were sent for routine investigations, which were as follows: Hemoglobin was 14.2 g/dL, thyroid profile was within normal range, bleeding time and clotting time were also within normal limits, random blood sugar was 105 mg/dL and the reverse transcriptase polymerase chain reaction (RT-PCR) test for COVID-19 was negative. The patient underwent bilateral tonsillectomy under general anesthesia.
Post-tonsillectomy, the tonsils were sent for histopathological examination.
The gross pictures of the specimen as shown in Figures 2 and 3 were rather surprising as they showed pus in the tonsil parenchyma, which went in favor of diagnosis of “intratonsillar abscess”, and the microscopic findings too confirmed the diagnosis of “intratonsillar abscess” (Figs. 4 and 5).

Figure 2. Gross picture of left-sided tonsil with pus within the tissue measuring 2.5 × 1.5 × 1 cm.

Figure 3. Cut section shows yellowish fluid filled within cystic cavity.
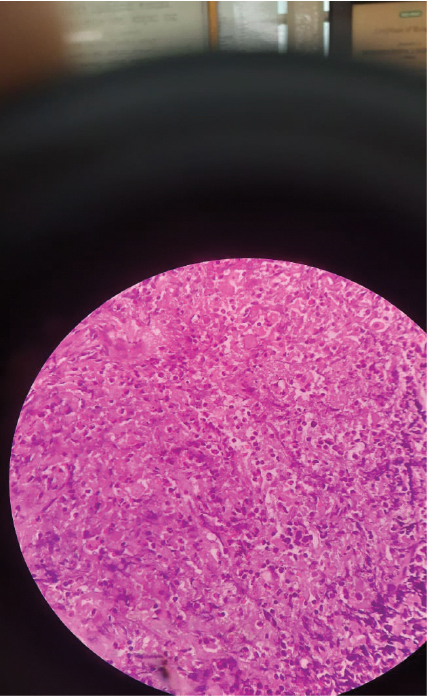
Figure 4. Microscopic picture showing numerous neutrophils.
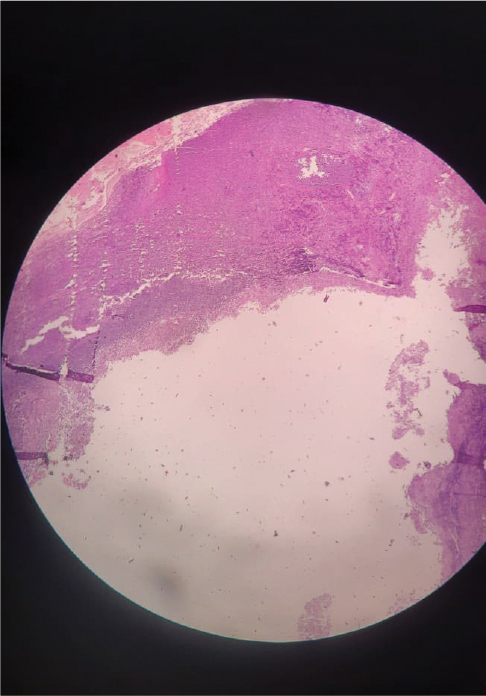
Figure 5. Cut section of left tonsil showing tonsillar tissue composed of lymphoid tissue lined by stratified squamous epithelium and cavity lined by inflammatory cells mainly neutrophils, lymphocytes, plasma cells and macrophages.
DISCUSSION
The palatine tonsils are a part of the Waldeyer’s lymphatic ring. They are located between the palatoglossal muscles anteriorly, palatopharyngeus muscle posteriorly and superior pharyngeal constrictor muscle laterally.
The tonsils are covered by fibrous sheath of connective tissue and nonkeratinized squamous epithelium. Tonsils have crypts in their structure, the largest crypt is magna crypta or intratonsillar cleft.
The superior pharyngeal constrictor helps in the contraction of the tonsillopharyngeus muscle facilitating the expulsion of the crypt contents.
Michaels and Hellquist2 suggested that when and if a suppurative focus arises in a case of acute tonsillitis and the outward drainage is prevented; a block in the crypt causes the pus to go inwards leading to an intratonsillar abscess.
The low incidence of intratonsillar abscess is due to the absence of lymphatic valves3 prior to the capsule, which does not allow aggregation of bacteria in the tonsillar tissue. Therefore, conditions affecting lymphatic flow such as dehydration or a previous history of peritonsillar abscess could lead to intratonsillar abscess.
Due to its gross appearance, an intratonsillar abscess could be mistaken for a tonsillolith.
As the abscess causes unilateral tonsillar enlargement, malignancy should be kept in mind, most commonly lymphoma.
Misdiagnosis of an intratonsillar abscess may lead to overuse of antibiotics leading to risk of antibiotic resistance.
Although a computed tomography (CT) scan is usually recommended for cases of intratonsillar abscess, it was not performed in this particular case because the differential diagnosis did not require it. However, a CT scan can be helpful in diagnosing an intratonsillar abscess as it would reveal a low-density and ring enhancement.
Management of any abscess requires early drainage. The preferred mode of treatment according to most studies is aspiration using a large bore needle, but needle aspiration requires repeated sittings and more importantly, the patient’s cooperation.
Review of medical literature reveals that few patients after repeated aspirations underwent tonsillectomy,5 which was also done in our case.
CONCLUSION
Intratonsillar abscess is a rare condition, and an accurate diagnosis can be challenging for otorhinolaryngologists.
In this particular case, a CT scan was not advised for the patient as the differential diagnosis did not warrant it. The patient underwent tonsillectomy as a treatment modality, although aspiration is also a viable treatment option if the patient is compliant with the procedure. As with any medical condition, careful consideration of the patient’s individual circumstances and medical history is necessary to determine the best course of treatment.
REFERENCES
- Esmaili A, Hasan Z, Friedland P. A review and report of a rare clinical entity: intratonsillar abscess. Otolaryngol Case Rep. 2018;6:43-6.
- Michaels, Leslie & Hellquist, Henrik. (2001). Ear, Nose and Throat Histopathology. 10.1007/978-1-4471-0235-9.
- Blair AB, Booth R, Baugh R. A unifying theory of tonsillitis, intratonsillar abscess and peritonsillar abscess. Am J Otolaryngol. 2015;36(4):517-20.
- Gan EC, Ng YH, Hwang SY, Lu PK. Intratonsillar abscess: a rare cause for a common clinical presentation. Ear Nose Throat J. 2008;87(12):E9.
- Wang AS, Stater BJ, Kacker A. Intratonsillar abscess: 3 case reports and a review of the literature. Int J Pediatr Otorhinolaryngol. 2013;77(4):605-7.