https://doi.org/10.59793/ijcp.v34i2.453
Abstract
The purpose of monitoring of the patient in an intensive care unit (ICU) is to improve patient care, like bringing about a change in the treatment or transfer of the patient to a step-down unit. Monitoring also shows the extent of compliance with a formulated standard of care or the degree of deviation from the expected standard of care. The monitoring used for a patient admitted to an ICU can be invasive or noninvasive. Invasive monitoring in an ICU includes arterial blood pressure, transesophageal Doppler, central venous pressure (CVP) measurement, pulmonary artery catheterization, arterial blood gas (ABG) analysis and measurement of intracranial pressure (ICP) and intra-abdominal pressure (IAP). Monitoring of the physiologic parameters depends on the underlying illness of the patient and the availability of equipment in the ICU.
Keywords: Invasive monitoring, intensive care unit
Patients admitted to an intensive care unit (ICU) require constant and intensive monitoring of their vital parameters. This helps in deciding about the future management of patients who have been stabilized and in modification of treatment in the acutely ill, unstable patient.
The components of invasive monitoring in the ICU are as follows:
- Invasive blood pressure (BP) monitoring
- Transesophageal Doppler (TED)
- Measurement of central venous pressure (CVP)
- Pulmonary artery catheterization
- Arterial blood gas (ABG) analysis
- Intracranial pressure (ICP) measurement
- Intra-abdominal pressure (IAP) measurement.
Invasive BP monitoring1
Indications
Continuous ‘beat-to-beat’ BP monitoring is useful in patients receiving inotropic drugs and head injury patients. Both groups of patients require close control of BP, which can be achieved by this technique.
Advantages
This method can be used in patients with gross peripheral edema, morbidly obese patients, patients in shock and patients who require repeated ABG analysis. It also allows measurement of cardiac output by pulse contour analysis of arterial pressure waveform.
The origin of pulse contour method of measuring cardiac output is derived from variations in the pulse pressure waveform. Pulse pressure is directly proportional to stroke volume and inversely related to vascular compliance. Pulse contour analysis is calibrated to injection dilution method. Stroke volume is calculated and compared with stroke volume as determined by the dilution technique; and the cardiac output is then calculated. With beat-to-beat waveform analysis, cardiac output can be determined continuously. Lithium is the contrast agent most commonly used with the injection dilution method for external calibration of pulse contour analysis devices (lithium indicator cardiac output [LiDCO], pulsed-induced contour cardiac output [PiCCO]).
Lithium indicator dilution cardiac output2
It is a minimally invasive technique of arterial pulse analysis that allows continuous, real-time cardiovascular monitoring. It is safe, accurate and simple to use. It is contraindicated in patients with intracardiac shunts, patients with atrial fibrillation and those on lithium therapy or patients receiving muscle relaxants.
Pulse-induced contour cardiac output
it is a pulse contour analysis with intermittent thermodilution measurement that enables continuous hemodynamic monitoring using femoral or axillary artery catheter.
Complications
- Infection (But less frequent than venous lines)
- Local thrombosis
- Damage to local nerves
- Bleeding/hematoma formation
- Pseudoaneurysm formation
TransEsophageal Doppler2
TED measures blood flow velocity in the descending aorta by a Doppler transducer (4 MHz continuous wave or 5 MHz pulsed wave) placed at the tip of a flexible probe. It estimates preload, myocardial contractility and vascular tone. A study has found 86% correlation between cardiac outputs as determined by esophageal Doppler and pulmonary artery catheterization.
Advantages
- Minimally invasive
- Can be inserted rapidly
- Allows real-time measurement
Limitations
Interference occurs by nasogastric tube.
- Can get dislodged by movement which may result in loss of signal.
- Inability to obtain continuous reliable measurements of hemodynamic parameters.
Central Venous Cannulation
Indications
- Patients requiring rapid resuscitation by infusion of fluids or blood.
- Patients requiring measurement of CVP.
- Patients requiring long-term drug administration.
- Patients undergoing hemodialysis.
- Patients undergoing plasmapheresis.
- Patients requiring placement of pacemaker.
Complications
- Immediate: Bleeding, arrhythmia, air embolism and pneumothorax.
- Delayed: Infection and venous thromboembolism.
Pulmonary Artery Catheterization3
Flow-directed pulmonary artery catheters, also called Swan-Ganz catheters are used in the diagnosis and management of a range of conditions in critically ill patients. Pulmonary artery catheterization can yield direct measurements of central venous, right-sided intracardiac, pulmonary arterial and pulmonary capillary wedge pressures.
Automated thermodilution techniques can be used to estimate cardiac output. Systemic and pulmonary vascular resistance can be calculated on the basis of vascular pressures and cardiac output.
Indications
Despite the widespread use of pulmonary artery catheters in hemodynamically unstable patients, no study has definitively demonstrated improved outcome in critically ill patients managed using pulmonary artery catheterization. Role of invasive hemodynamic monitoring in critically ill patients is controversial as the pulmonary artery catheter is yet to be proven to improve patient outcome.
Accepted indications for pulmonary artery catheterization have been generated largely on the basis of clinical experience. The decision to place a pulmonary artery catheter should be based upon a specific question regarding a patient’s hemodynamic status that cannot be answered satisfactorily by clinical or noninvasive assessment.
If the answer could change management, then placement of the catheter is indicated.
Diagnostic Uses
- To differentiate between mechanisms of pulmonary edema (cardiogenic and noncardiogenic).
- To diagnose left-to-right intracardiac shunt.
- To measure intracardiac pressures.
Therapeutic Uses
- Management of perioperative patient with unstable cardiac status.
- Management of patients following cardiac surgery.
Complications
There are three categories of complications related to the use of pulmonary artery catheters:
- Complications related to insertion of the pulmonary artery catheter.
- Sustained ventricular arrhythmias occur in up to 3% of patients.
- Right bundle branch block (RBBB) develops during approximately 5% of catheter insertions.
Complications related to maintenance and use of catheter
- pulmonary artery perforation is the most feared complication. It has a mortality of more than 30% and usually requires emergent thoracotomy for management. Self-limited pulmonary hemorrhage following perforation can result in the formation of a pulmonary artery pseudoaneurysm. Risk factors for pulmonary artery rupture are pulmonary hypertension, advanced age, mitral valve disease, hypothermia and anticoagulant therapy.
- Migration of the catheter may result in pulmonary infarction.
- Thromboembolic events may occur with catheters acting as a nidus for thrombus formation.
- Catheter-related infections with possible bloodstream infection.
Complications related to data interpretation
under ideal conditions, the tip of the catheter sits in zone 3 of the lung, where the arterial pressure exceeds the venous pressure and the venous pressure exceeds the alveolar pressure, thereby creating a continuous column of blood from the catheter tip to the left atrium (LA) when the balloon is inflated. Also, the LA pressure is similar to left ventricular end-diastolic pressure (LVEDP).
These conditions may not necessarily apply in many settings, and can result in hemodynamic data, which can be inaccurate. Sources of error are improperly calibrated pressure monitors, transduction of airway pressures under non-zone 3 conditions and over estimation of pulmonary capillary wedge pressure (PCWP) due to incomplete pulmonary artery branch occlusion. Also, interobserver variability in the interpretation of hemodynamic data among ICU physicians and anesthesiologists can lead to misinterpretation of accurately measured data.
ABG Analysis
Analysis of ABG gives an idea about the oxygenation status and allows the clinician to assess the elimination of carbon dioxide and metabolic parameters of the critically ill patient. The information obtained from ABG analysis allows better goal directed management of the ICU patient.
Parameters reflected in the ABG report are pH, PO2, PCO2, SaO2, bicarbonate (HCO3–) and base excess.4
- pH: Normal arterial blood pH is 7.35-7.45. pH <7.35 indicates acidosis and pH >7.45 indicates alkalosis.
- PO2: Normal range is 75-100 mmHg. Values of PO2 <60 indicate the need for mechanical ventilation in the patient.
Conditions with low PO2 in ICU are:4 Hypoventilation, impaired diffusion, ventilationperfusion mismatch and shunting.
PaO2/FiO2 ratio (P/F):4 Normal ratio >500
Ratio between 300-500 – Mild hypoxemia
Ratio between 200-300 – Acute lung injury (ALI)
Ratio <200 – Acute respiratory distress syndrome (ARDS).
PaO2/FiO2 ratio (P/F) is used for evaluating the severity of lung involvement in ALI/ARDS.4
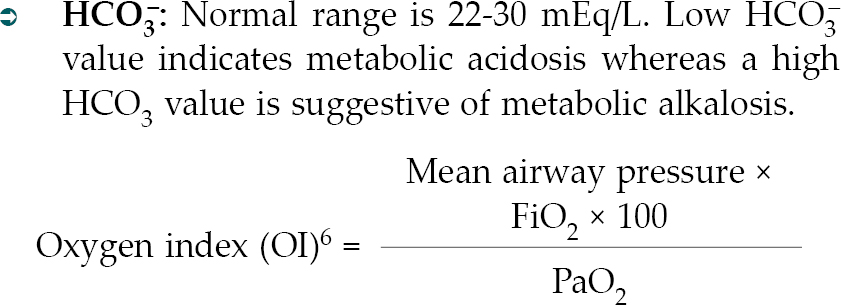
Oxygen index (OI) accounts better for the influence of ventilator pressures on oxygenation value. In patients with ARDS, OI >8.1 is usually in agreement with P/F <200. However, patients with ALI having an OI of 5.3-08.1 frequently had P/F <200.5
- PCO2: Normal range is 35-45 mmHg. A high value is indicative of respiratory acidosis and suggests hypoventilation, while a low value indicates respiratory alkalosis due to hyperventilation.
- SaO2: Normal range is 95-100.
- Base excess (BE): Normal range is –2 to +2 mEq/L. BE may indicate tissue acidosis. But, it is a crude indicator of tissue dysoxia. Tissue hypoperfusion may occur in the absence of a significant change in the BE.7
ICP Monitoring
Normal ICP is in the range of 10-15 mmHg.
Indications for ICP Monitoring
- Head injury
- Intracerebral hemorrhage
- Subarachnoid hemorrhage
- Hydrocephalus
- Cerebrovascular stroke
- Cerebral edema
- Brain tumors
Devices for ICP Monitoring
- Intraventricular catheter (Gold Standard)
- Epidural catheter
- Subdural catheter
Measurement of ICP is useful in the calculation of cerebral perfusion pressure (CPP).
CPP = Mean arterial BP-ICP.
Normally, CPP is more than 60 mmHg.
Newer Fiberoptic ICP Monitors8
Advantages
- They have a smaller diameter, so they cause less damage to brain tissue.
- Allow simultaneous measurement of ICP and local cerebral blood flow by using Doppler flowmetry.
- Also measure brain tissue oxygen pressure, CO2 pressure, pH and other metabolic parameters.
Disadvantages
- Cannot be used for cerebrospinal fluid (CSF) drainage.
- Cannot be recalibrated in situ.
IAP Monitoring
Studies have shown that there is no correlation between abdominal girth and IAP measurements. Sensitivity of physical examination for intra-abdominal hypertension has been estimated to be 40% to 60% approximately. Normal IAP value ranges between 0 and 5 mmHg. Direct measurements of IAP with an intraperitoneal catheter are precise. However, the less invasive and inexpensive technique of intravesical manometry is the recommended standard.
There are 4 grades of intra-abdominal hypertension:
- Grade I: IAP is between 12-15 mmHg
- Grade II: IAP is between 16-20 mmHg
- Grade III: IAP is between 21-25 mmHg
- Grade IV: IAP is >25 mmHg.
Indications
- Severe acute pancreatitis.
- Intra-abdominal bleeding (rupture of abdominal aortic aneurysm).
The risk of developing intra-abdominal hypertension is minimal in:9
Mechanically ventilated patients with positive endexpiratory pressure (PEEP) <10 cm H2O and PaO2/FiO2 ratio >300.
- Patients with body mass index (BMI) <30 kg/m².
- Patients without pancreatitis, hepatic failure, cirrhosis of liver with ascites, gastrointestinal bleeding or in patients undergoing laparotomy and the use of vasopressors/inotropes on admission.
Presently, there are no clear guidelines to select the patients in whom IAP measurements should be performed.9
CONCLUSION
In critical care, monitoring is essential in the daily care of ICU patients as the optimization of the patient’s hemodynamic parameters, ventilation, temperature and metabolism is the key to improving patients’ survival.
REFERENCES
- Gupta B. Update in Anaesthesia. Vol. 21, World Federation of Society of Anaesthesiologists. December 2007.
- Marik PE, Baram M. Non-invasive hemodynamic monitoring in the intensive care unit. Crit Care Clin. 2007;23:383-400.
- Weinhouse GL. Pulmonary artery catheterization: indications and complications. In: UpToDate, Basow DS (Ed.), UpToDate. Waltham, MA; 2012.
- Kipnis E, Ramsingh D, Bhargava M, Dincer E, Cannesson M, Broccard A, et al. Monitoring in the intensive care. Crit Care Res Pract. 2012;2012:473507.
- Van Haperen M, Van der Voort PH, Bosman RJ. The Oxygenation Index compared with the P/F ratio in ALI/ARDS. Crit Care. 2012;16(Suppl 1):91.
- Brochard L, Martin GS, Blanch L, Pelosi P, Belda FJ, Jubran A, et al. Clinical review: Respiratory monitoring in the ICU - a consensus of 16. Crit Care. 2012;16(2):219.
- Marik PE. The optimal endpoint of resuscitation in trauma patients. Crit Care. 2003;7(1):19-20.
- Invasive monitoring in an intensive care unit. In: Grover A, Aggarwal V, Gera P, Gupta R, (Eds.). Manual of Medical Emergencies. 3rd Edition, New Delhi: Pushpanjali Medical Publications Pvt. Ltd.; 2007. p. 40.
- Starkopf J, Tamme K, Blaser AR. Should we measure intra-abdominal pressures in every intensive care patient? Ann Intensive Care. 2012;2 Suppl 1:S9.