https://doi.org/10.59793/ijcp.v34i8.760
Abstract
Background: Iron deficiency during pregnancy is one of the primary causes of anemia in infants and young children. It has a negative impact on maternal and fetal health throughout pregnancy with higher likelihood of adverse maternal and fetal outcomes. Maternal iron supplementation is a critical tool to address the global problem of iron deficiency and prevent its negative consequences. Method: An open-label non-comparative prospective clinical trial was carried out to evaluate the effectiveness of “Sangfer” liquid in 16 pregnant women with anemia. “Sangfer” is a polyherbal Ayurvedic proprietary medication containing elemental iron and zinc and four medicinal herbs viz. Withania somnifera, Emblica officinalis, Asparagus racemosus and Pueraria tuberosa. The aim of the study was to examine its efficacy and safety in treating anemia in pregnant women. The dose administered was 10 mL twice daily after food for 12 weeks (84 days). Patients were evaluated at screening (Visit 1 at Day 0), baseline (Visit 2 at Day 1) and during follow-ups (Visit 3 at Day 28, Visit 4 at Day 56 and Visit 5 at Day 84). Results: There was a significant increase in mean hemoglobin levels from 8.08% at Day 1 to 11.19% at the final visit at Day 84. The anemia sign and symptom scores also significantly reduced from Day 1 to different follow-up visits. The mean Physician Global Assessment (PGA) score was found to reduce from 1.0 at Day 1 to 0.0 at the final follow-up visit. Conclusion: “Sangfer” is highly effective for the treatment of anemia during pregnancy. No adverse effects including serious adverse effects were observed during the study period.
Keywords: Iron deficiency anemia, pregnancy, liquid, medicinal herbs, hemoglobin, anemia sign and symptom scores
Iron deficiency anemia (IDA) is very common, particularly in underdeveloped countries, and is now reaching a state of pandemic.1 Iron deficiency during pregnancy is one of the primary causes of anemia in infants and young children.2 Pregnancy increases iron demand, which increases the risk of anemia. It has a negative impact on maternal and fetal health throughout pregnancy, and has been associated with higher morbidity and fetal mortality.3 Breathing difficulties, fainting, fatigue, palpitations and sleep problems are common among affected mothers.4 They are also more likely to have perinatal infection, pre-eclampsia and bleeding. There are also concerns of postpartum cognitive decline and behavioral difficulties.5,6 Anemia during pregnancy is also associated with poor perinatal outcomes such as preterm labor, intrauterine growth retardation, low birth weight, birth asphyxia and neonatal anemia.7,8 Maternal iron supplementation is a critical tool to address the global problem of iron deficiency and prevent its negative consequences.9 Since ancient times, numerous iron formulations have been empirically used in the treatment of anemia in Ayurveda.10
In this study, an Ayurvedic proprietary medication “Sangfer” containing elemental iron and zinc and four medicinal herbs Withania somnifera, Emblica officinalis, Asparagus racemosus and Pueraria tuberosa was investigated for its efficacy in the treatment of anemia in pregnant women.
Therefore, an open-label non-comparative prospective clinical trial was carried out to assess the effectiveness of “Sangfer” liquid in pregnant female participants with anemia.
STUDY OBJECTIVES
Primary Objective
The primary objective of this study was to evaluate the efficacy of “Sangfer” liquid in anemia in pregnant women.
Secondary Objective
The secondary objective was to assess the tolerability of the supplement in study participants.
STUDY DESIGN
This study was an open-label, single-arm, non-comparative prospective clinical study to evaluate the efficacy and tolerability of “Sangfer” liquid in pregnant women suffering from anemia. The 84-day study duration consisted of five assessment points, including screening (Visit 1, Day 0), baseline (Visit 2, Day 1), two follow-ups (Visits 3 and 4, Days 28 and 56, respectively) and final visit (Visit 5, Day 84). After receiving informed consent, subjects were evaluated for eligibility based on inclusion and exclusion criteria.
After baseline assessment at Visit 2, “Sangfer” liquid was given to all eligible subjects. Subjects were instructed to take the liquid 10 mL twice daily after food for 84 days (12 weeks).
STUDY POPULATION
Pregnant women with anemia were recruited from the outpatient clinic. Potential subjects were identified by the site investigator or by designated physician based on the inclusion and exclusion criteria. A total of 16 subjects were recruited for this study.
Inclusion Criteria
Subjects who met all of the following criteria were included in the study:
- Pregnant women aged between 18 to 35 years.
- Subjects up to the 7th month of pregnancy with a clinical diagnosis and laboratory confirmation of anemia, but with hemoglobin level not <8 g/dL.
- Subjects with hemoglobin level ≤10 g/dL and peripheral blood imaging showed microcytic, normocytic and hypochromic red blood cells.
- Subjects who were able to understand the risks/benefits of the protocol.
- Subjects who gave their written informed consent and agreed to come for regular follow-up.
Exclusion Criteria
Subjects who met any of the following criteria were excluded from the study:
- Participants with hemoglobin level ≤8 g/dL.
- Participants with a history of anemia due to any bleeding condition such as bleeding hemorrhoids, menorrhagia (cyclical vaginal bleeding excessive in quantity or duration), gastric ulcers, etc.
- Individuals with bleeding disorders such as coagulation defects, thalassemia, etc.
- Presence of any other comorbid disease such as renal failure, coronary disease, hypertension, tuberculosis, diabetes mellitus, etc.
- Subjects with history of thyroid dysfunction.
- History of psychiatric disorder that could affect subjects’ ability to give written informed consent.
- Subjects with a history of stroke, myocardial infarction, coronary artery disease, heart failure, angina, life-threatening arrhythmia in the past 6 months.
- Subjects with uncontrolled diabetes (fasting blood sugar >140 mg/dL) and high blood pressure >130/90 mmHg.
- Subject with acquired immunodeficiency syndrome (AIDS) or history of any other sexually transmitted diseases (STDs).
- Subjects with high alcohol consumption (>2 standard drinks per day), smokers and recreational drug use (such as cocaine, methamphetamine, marijuana, etc.)/nicotine/caffeine dependence.
- Subjects who had participated in a clinical study in the last 30 days prior to entering this study.
STUDY PRODUCT DETAILS
The study product “Sangfer” is a proprietary Ayurvedic oral liquid for the treatment of anemia in pregnant women. “Sangfer” liquid contains medicinal plants (W. somnifera, E. officinalis, A. racemosus and P. tuberosa) used in Ayurvedic medicines.
CONCOMITANT THERAPY
No concomitant medication was allowed during the study. However, if participants reported any clinical symptoms during the study, the study physician prescribed the appropriate medication, which was documented.
STUDY ENDPOINTS
Primary Endpoint
- The primary endpoint included the mean change in hemoglobin level from baseline to the end of the study.
Secondary Endpoints
The secondary endpoints were included:
- Mean change in the global assessment on overall improvement by the investigator and by the patient from baseline to the end of the study.
- Change in subjective scores in the improvement of weakness (Daurbalya), fatigue (Shrama), breathlessness (Shwasa), pallor – skin, face, sclera, nails (Pandu Varna Twak, etc.) from baseline to the end of the study.
- Mean changes in vital sign parameters from baseline to end of study.
- Frequency and severity of the occurrence of adverse events during the treatment period.
- Proportion of subjects who discontinued study treatment due to adverse events.
STUDY ASSESSMENTS
Visit 1 (Screening): Screening events were performed at Visit 1 (Day 0). Potential subjects were identified and written informed consent was obtained from all participants. Eligible subjects meeting the entry criteria were enrolled in the study. All subjects were assessed for physical examinations, vital signs, demographic data, medical histories, including concomitant medications.
Visit 2 (Baseline): Baseline data was evaluated at Visit 2 (Day 1). During this visit, all subjects underwent physical examination, vital signs, concomitant medications, blood test for hemoglobin level, anemia sign and symptoms (weakness, fatigue, breathlessness and pallor) scores and Physician Global Assessment (PGA) score.
Visit 3 (Follow-up): All participants underwent a medical assessment during Visit 3. At this visit, all subjects were assessed for the physical examination, vital signs, concomitant medications, adverse events, blood test for hemoglobin level, IDA sign and symptoms scores and PGA score.
Visit 4 (Follow-up): All participants underwent a medical assessment during this visit (Day 56). They underwent physical examination and were assessed for vital signs, concomitant medications, adverse events, blood test for hemoglobin level, IDA sign and symptoms scores and PGA score.
Visit 5 (End of the Study): All participants underwent a medical assessment during this visit (Day 84). At this visit, physical examination and assessment of vital signs, concomitant medications, adverse events, blood test for hemoglobin level, IDA sign and symptoms scores and PGA score were done.
STATISTICAL PLANS
Data were abstracted and presented as number, percentage, mean and standard deviation (SD). All efficacy and safety variables were summarized using descriptive statistics. Data comparison between baseline and follow-up visits was performed using paired t-test or one-way analysis of variance (ANOVA), as appropriate, and data were expressed as mean, SD, 95% confidence interval (CI) and p-value. A p value of 0.05 was considered statistically significant. Statistical analysis was done using statistical software SPSS 10.0.
RESULTS
Data Sets Analyzed
A total of 18 female subjects were screened for eligibility; 16 subjects enrolled in the study and 2 subjects were screening failures. All subjects were given the test product “Sangfer” liquid and instructed to take 10 mL liquid twice daily after meal for 84 days. All 16 subjects completed the study, and hence, the data of 16 subjects was analyzed for this study.
Demographic Data
The mean age of the participants was 23.94 ± 2.93 years. The maximum age enrolled was 31 years, and the minimum age enrolled was 20 years. The mean weight of the participants was 47.75 ± 2.89 kg.
Efficacy Assessment
Assessment of hemoglobin level
Hemoglobin levels were evaluated at Day 1 (V2) through Days 28 (V3), 56 (V4) and 84 (V5) (Table 1). Results showed a significant increase in the mean hemoglobin levels from Day 0 to different follow-up visits. Mean changes in hemoglobin levels on Days 56 and 84 were found to be statistically significant (p < 0.0001) compared to Day 1 (Table 2 and Fig. 1).
|
Table 1. Mean Hemoglobin Level at Different Visits
|
|
Parameters
|
Visit (V)
|
Mean (n = 16)
|
SD
|
|
Hemoglobin (g/dL)
|
Baseline (V2, Day 1)
|
8.08
|
0.39
|
|
Follow-up (V3, Day 28)
|
8.42
|
0.39
|
|
Follow-up (V4, Day 56)
|
9.36
|
0.55
|
|
Final visit (V5, Day 84)
|
11.19
|
0.67
|
|
Table 2. Comparison of Mean Change in Hemoglobin Level from Day 0 to Different Follow-up Visits
|
|
Parameters
|
Visit (V)
|
Mean score (mean ± SD)
|
Change from V1 (mean ± SD)
|
95% CI of Diff.
|
P value
|
|
Hemoglobin (g/dL)
|
V2
|
8.08 ± 0.39
|
-
|
-
|
<0.0001
|
| |
V3
|
8.42 ± 0.39
|
0.34 ± 0.20
|
−0.8414 to 0.1539
|
|
| |
V4
|
9.36 ± 0.55
|
1.29 ± 0.51***
|
−1.785 to −0.7898
|
|
| |
V5
|
11.19 ± 0.67
|
3.11 ± 0.66***
|
−3.610 to −2.615
|
|
Mean hemoglobin at Day 1 (V2) was compared with Days 28 (V3), 56 (V4) and 84 (V5) by one-way ANOVA test. Comparison: V2 vs. V3, V4 and V5. Level of significance ***p < 0.0001.
*P < 0.05, **P < 0.01, ***P < 0.001.
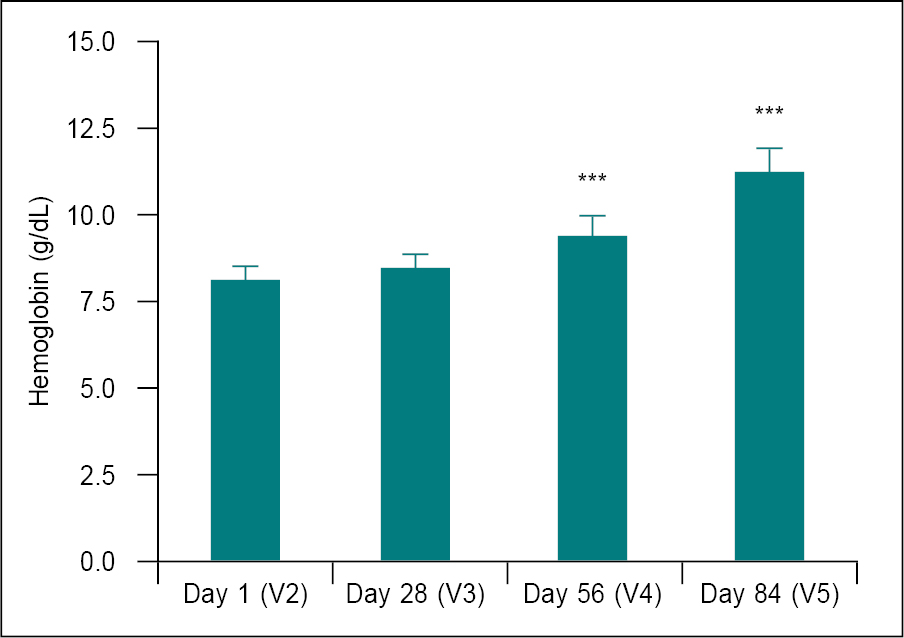
Figure 1. Comparison of mean change in hemoglobin level from Day 1 (V2) to different follow-up visits (n = 16).
Mean of hemoglobin at V2 was compared with Visits V3, V4 and V5 using one-way ANOVA. Comparison: V2 vs. V3, V4 and V5. Significance level ***p < 0.0001.
*P < 0.05, **P < 0.01, ***P < 0.001.
Assessment for anemia signs and symptoms
Anemia sign and symptom scores were assessed at Days 1 (V2), 28 (V3), 56 (V4) and 84 (V5) (Table 3). Results showed a significant reduction in anemia sign and symptom scores from Day 1 (V2) to different follow-up visits. Mean changes in all anemia sign and symptom scores (except weakness score at Day 28) were found to be statistically significant (p < 0.0001) from Day 28 (V3) onwards compared to Day 1 (V2) (Table 4). Reduction in weakness score was found to be statistically significant (p < 0.0001) from Day 56 (V4) onwards.
|
Table 3. Means of Anemia Sign and Symptom Scores at Different Visits
|
|
Parameters
|
Visit (V)
|
Mean (n = 16)
|
SD
|
|
Weakness
|
V2 (Day 1)
|
1.0
|
0.00
|
|
V3 (Day 28)
|
0.73
|
0.46
|
|
V4 (Day 56)
|
0.19
|
0.40
|
|
V5 (Day 84)
|
0.0
|
0.0
|
|
Fatigue
|
V2 (Day 1)
|
1.0
|
0.0
|
|
V3 (Day 28)
|
0.56
|
0.51
|
|
V4 (Day 56)
|
0.0
|
0.0
|
|
V5 (Day 84)
|
0.0
|
0.0
|
|
Breathlessness
|
V2 (Day 1)
|
1.0
|
0.0
|
|
V3 (Day 28)
|
0.50
|
0.52
|
|
V4 (Day 56)
|
0.0
|
0.0
|
|
V5 (Day 84)
|
0.0
|
0.0
|
|
Pallor
|
V2 (Day 1)
|
1.0
|
0.0
|
|
V3 (Day 28)
|
0.38
|
0.50
|
|
V4 (Day 56)
|
0.0
|
0.0
|
|
V5 (Day 84)
|
0.0
|
0.0
|
|
Table 4. Comparison of Mean Change in Anemia Symptom Scores from Baseline to Different Follow-up Visits (n = 16)
|
|
Parameters
|
Visit (V)
|
Mean score (mean ± SD)
|
Change from V1 (mean ± SD)
|
95% CI of Diff.
|
|
Weakness
|
V2
|
1.0 ± 0.0
|
-
|
-
|
|
V3
|
0.73 ± 0.46
|
0.31 ± 0.48
|
−0.029 to 0.563
|
|
V4
|
0.19 ± 0.40
|
0.81 ± 0.40***
|
0.521 to 1.104
|
|
V5
|
0.0 ± 0.0
|
1.0 ± 0.0***
|
0.709 to 1.291
|
|
Fatigue
|
V2
|
1.0 ± 0.0
|
-
|
-
|
|
V3
|
0.56 ± 0.51
|
0.44 ± 0.51***
|
0.190 to 0.685
|
|
V4
|
0.0 ± 0.0
|
1.0 ± 0.0***
|
0.753 to 1.247
|
|
V5
|
0.0 ± 0.0
|
1.0 ± 0.0***
|
0.753 to 1.247
|
|
Breathlessness
|
V2
|
1.0 ± 0.0
|
-
|
-
|
|
V3
|
0.5 ± 0.52
|
0.50 ± 0.52***
|
0.251 to 0.749
|
|
V4
|
0.0 ± 0.0
|
1.0 ± 0.0***
|
0.751 to 1.249
|
|
V5
|
0.0 ± 0.0
|
1.0 ± 0.0***
|
0.751 to 1.249
|
|
Pallor
|
V2
|
1.0 ± 0.0
|
-
|
-
|
|
V3
|
0.38 ± 0.50
|
0.63 ± 0.50***
|
0.384 to 0.866
|
|
V4
|
0.0 ± 0.0
|
1.0 ± 0.0***
|
0.759 to 1.241
|
|
V5
|
0.0 ± 0.0
|
1.0 ± 0.0***
|
0.759 to 1.241
|
IDA sign and symptom scores at baseline (V2) were compared with follow-up visits (V3, V4 and V5) using one-way ANOVA. Comparison: V2 vs. V3, V4 and V5. Significance level ***p < 0.001.
*P < 0.05, **P < 0.01, ***P < 0.001.
Assessment of PGA
Assessment of PGA score was assessed at all assessment points (Table 5). Results showed that the PGA score was significantly (p < 0.001) reduced at Days 28, 56 and 84 compared to Day 1 (Table 6 and Fig. 2).
|
Table 5. Means of PGA Scores at Different Visits
|
|
Assessment
|
Visit (V)
|
Mean (n = 16)
|
SD
|
|
PGA score
|
V2
|
1.0
|
0.0
|
|
V3
|
0.31
|
0.48
|
|
V4
|
0.0
|
0.0
|
|
V5
|
0.0
|
0.0
|
|
Table 6. Comparison of Mean Change in PGA Score from Baseline to Different Follow-up Visits (n = 16)
|
|
Assessment
|
Visit (V)
|
Mean score (mean ± SD)
|
Change from V1 (mean ± SD)
|
95% CI of Diff.
|
|
PGA score
|
V2
|
1.0 ± 0.0
|
-
|
-
|
|
V3
|
0.31 ± 0.48
|
0.69 ± 0.48***
|
0.457 to 0.918
|
|
V4
|
0.0 ± 0.0
|
1.0 ± 0.0***
|
0.769 to 1.231
|
|
V5
|
0.0 ± 0.0
|
1.0 ± 0.0***
|
0.769 to 1.231
|
PGA score at Day 1 (V2) were compared with follow-up visits (V3, V4 and V5) using one-way ANOVA. Comparison: V2 vs. V3, V4 and V5. Significance level ***p < 0.001.
*P < 0.05, **P < 0.01, ***P < 0.001.
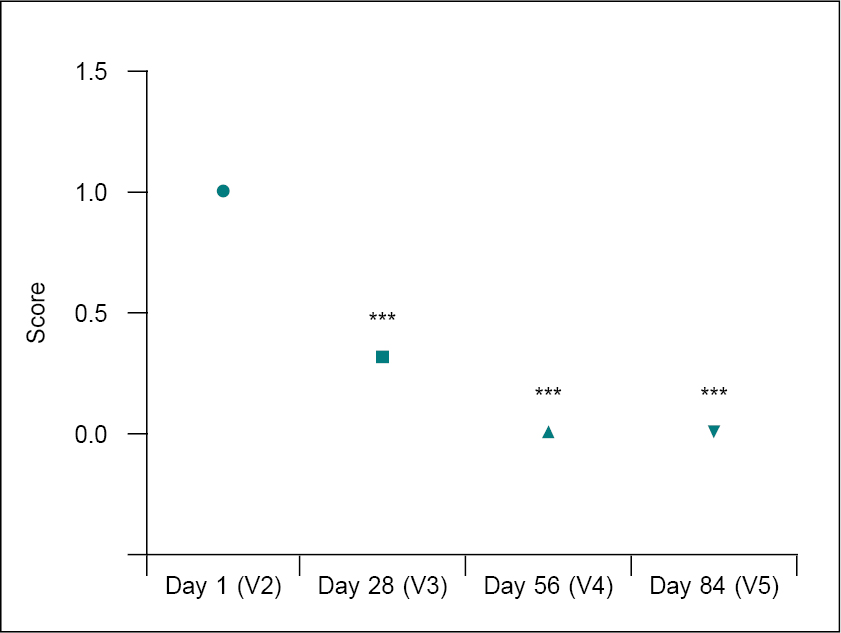
Figure 2. Comparison of mean change in PGA score from Day 1 (V2) to different follow-up visits (n= 16).
PGA score at V2 were compared with follow-up visits (V3, V4 and V5) using one-way ANOVA. Comparison: V2 vs. V3, V4 and V5. Significance level ***p < 0.001.
*P < 0.05, **P < 0.01, ***P < 0.001.
Safety Assessment
Assessment of general health symptoms
During the study period, the general appearance, eyes, ears, nose, throat, abdomen, heart and chest of all subjects were examined to look for any treatment-related abnormalities. No abnormalities were observed at any study visit.
Assessment of vital signs
Vital sign parameters of all subjects, including heart rate, systolic and diastolic blood pressure, were measured at all assessment points (Table 7). The baseline (Day 1, V2) vital signs data were compared to the Days 28 (V3), 56 (V4) and 84 (V5). There was no significant difference in vital sign parameters between Day 1 and Day 84; all values were within the normal range (Table 8 and Fig. 3).
|
Table 7. Mean Vital Signs at Different Visits
|
|
Parameters
|
Visits
|
Range
(Min. – Max.)
|
Mean (n = 16)
|
SD
|
|
Heart rate (bpm)
|
V2
|
72-86
|
81.56
|
3.52
|
|
V3
|
72-82
|
79.25
|
2.52
|
|
V4
|
80-82
|
80.75
|
1.0
|
|
V5
|
78-82
|
80.38
|
1.09
|
|
SBP (mm/Hg)
|
V2
|
100-120
|
110.63
|
4.43
|
|
V3
|
110-120
|
112.50
|
4.47
|
|
V4
|
100-120
|
110.0
|
5.16
|
|
V5
|
110-120
|
115.63
|
5.12
|
|
DBP (mm/Hg)
|
V2
|
70-80
|
72.50
|
4.47
|
|
V3
|
70-80
|
74.38
|
5.12
|
|
V4
|
70-80
|
76.25
|
5.0
|
|
V5
|
70-80
|
73.75
|
5.0
|
|
Table 8. Comparison of Mean Change in Vital Signs from Baseline to Different Follow-up Visits
|
|
Parameters
|
Visit (V)
|
Mean ± SD (n = 16)
|
Change from V1 (mean ± SD)
|
95% CI of Diff.
|
|
Heart rate (bpm)
|
V2
|
81.56 ± 3.52
|
-
|
-
|
|
V3
|
79.25 ± 2.52
|
−2.31 ± 4.35*
|
0.107 to 4.518
|
|
V4
|
80.75 ± 1.0
|
−0.81 ± 3.75
|
−1.393 to 3.018
|
|
V5
|
80.38 ± 1.09
|
−1.19 ± 3.78
|
−1.018 to 3.393
|
|
SBP (mm/Hg)
|
V2
|
110.63 ± 4.43
|
-
|
-
|
|
V3
|
112.50 ± 4.47
|
1.88 ± 6.55
|
−6.514 to 2.764
|
|
V4
|
110.0 ± 5.16
|
−0.63 ± 6.80
|
−4.014 to 5.264
|
|
V5
|
115.63 ± 5.12
|
5.0 ± 6.32*
|
−9.639 to −0.361
|
|
DBP (mm/Hg)
|
V2
|
72.50 ± 4.47
|
-
|
-
|
|
V3
|
74.38 ± 5.12
|
1.88 ± 7.5
|
−6.607 to 2.857
|
|
V4
|
76.25 ± 5.0
|
3.75 ± 8.06
|
−8.482 to 0.982
|
|
V5
|
73.75 ± 5.0
|
1.25 ±
7.19
|
−5.982 to 3.482
|
Vital signs data at Day 1 (V2) were compared to Days 28 (V3), 56 (V4) and 84 (V5) using the one-way ANOVA test. Comparison: V2 vs. V3, V4 and V5. Significance level *p < 0.05.
*P < 0.05, **P < 0.01, ***P < 0.001.
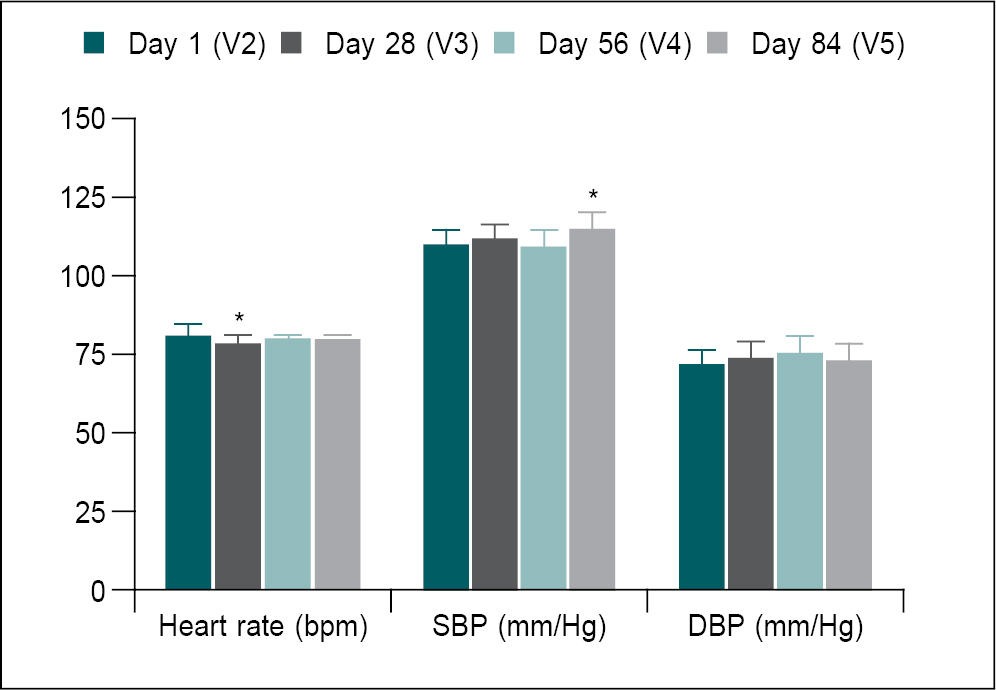
Figure 3. Comparison of mean change in vital signs from Day 1 (V2) to different follow-up visits.
Vital signs data at Day 1 (V2) were compared to Days 28 (V3), 56 (V4) and 84 (V5) using the one-way ANOVA test. Comparison: V2 vs. V3, V4 and V5. Significance level *p < 0.05.
*P < 0.05, **P < 0.01, ***P < 0.001.
Adverse events
No adverse effects including serious adverse effects were observed during the study period.
DISCUSSION
- somnifera or Ashwagandha is esteemed for its medicinal properties. It is commonly referred to as the “Indian Ginseng” due to its remarkable rejuvenating effects.11 W. somnifera has been classified as a Rasayana (rejuvenation) in Ayurveda.12 It is known to enhance vitality, energy, endurance and stamina, foster longevity and fortify the immune system, all without stimulating the body’s reserves.11 Studies have shown various properties of W. somnifera including antioxidant, anxiolytic, adaptogen, memory enhancing, antiparkinsonian, antivenom, sedative, diuretic, anti-inflammatory, antitumor and antistress properties.13
A study was conducted in anemic Albino Wistar rats to examine its antianemic activity. Following administration of the root extract of the herb, there was rapid and progressive recovery of the study animals due to the augmentation of erythropoiesis and defense against hemolysis caused by oxidative stress. The improvement in the hematological indices has been attributed to the iron content of the root extract. Iron plays a vital role in hemoglobin synthesis. These findings provide empirical support for the use of W. somnifera root extract in the treatment of anemia.14 The oral administration of a concentrated root extract of Ashwagandha at a high dosage was found to be associated with an elevation in maximal oxygen consumption (VO2 max) thereby improving cardiorespiratory endurance and enhancing quality of life in healthy athletic adults. Additionally, it was observed that Ashwagandha root extract positively influenced the red blood cell (RBC) count and hemoglobin levels. The increase in RBC count allows for improved oxygen transportation directly to the muscles during exercise, thus enhancing the athletes’ aerobic capacity. Overall, these findings propose a plausible mechanism for the ergogenic effect of Ashwagandha root extract.11,15
- officinalis, also known as Amla or Indian gooseberry, is a rich source of vitamin C. It is often used as a Rasayana in Ayurveda for the management of IDA (Pandu).16 The other major phytoconstituents of E. officinalis include polyphenols (gallic acid, ellagic acid), tannins and flavonoids (rutin and quercetin).17 It has antioxidant, immunomodulatory, antipyretic, analgesic, cytoprotective, memory-enhancing, antitussive, gastroprotective, purgative and spasmolytic properties.18,19
Phytates in food inhibit the absorption of dietary nonheme iron, whereas vitamin C enhances bioavailability of iron.16,20 The ascorbic acid enhances reduction of ferric iron to ferrous form leading to increase in iron absorption. It also prevents the inhibitory effect of phytates on iron absorption.21 The effect of the aqueous extract of fruit of E. officinalis on various hematological parameters was evaluated in Wistar albino rats. Following administration of the extract in doses of 250 mg/kg and 500 mg/kg body weight, a significant increase in packed cell volume, hemoglobin concentration, RBC, mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), mean corpuscular volume (MCV) and platelet count was observed compared to controls. The white blood cell (WBC) count also showed a marked increase at all doses administered. Other important findings of the study were reduction in total cholesterol and triglycerides.20,22
A study was conducted in a tertiary care teaching hospital, to assess the impact of amloki on RBC, WBC and platelet count. A total of 43 pregnant women aged 18 to 36 years, between the 13th and 20th weeks of gestation and diagnosed with IDA were selected for this study. The participants were divided into two groups: Group A, which received oral iron and amloki supplementation, and Group B, which received only iron supplementation, for a period of 45 days. A significant increase (p < 0.05) in RBC count was observed in both groups following iron intervention. Furthermore, the iron + amloki supplemented group demonstrated a significantly higher increase in RBC count compared to the group receiving only iron supplementation. This study also observed an increase in WBC count in the iron + amloki supplemented group and a decrease in platelet count in both groups, although these changes were not statistically significant. The study concluded that combination of oral iron and E. officinalis (amloki) supplementation leads to an increased blood RBC count in pregnant women with IDA.20
- racemosus or Shatavari is known as the “Queen of herbs” and is considered a health tonic and used as a rejuvenator. It improves longevity, vigor, mental function and boosts immunity. A. racemosus has antioxidant, anti-inflammatory, antiseptic and antimicrobial properties.23 It also has potent adaptogenic activity, which reduces stress and protects against infection and illness.24
A study was conducted with the chloroform:methanol (2:1) extract of A. racemosus in rats with experimentally induced anemia and thrombocytopenia. The doses used in the study were 250, 500 and 750 mg/kg given orally for a duration of 10 days. Oral administration of 750 mg/kg of the root extract resulted in substantial increase in the number of RBC and hemoglobin, while the MCH and total leukocyte count decreased. The bleeding and clotting time was also reduced in comparison to the heparin group. This study demonstrated that the root extract of A. racemosus possesses noteworthy antianemic and antithrombocytopenic properties.25
Traditionally, P. tuberosa is a restorative tonic and is used for its antiaging and health-promotive activities.26 It is an energizer, vital energy booster and immune booster.27 The tubers and leaves are rich in phytoconstituents for example, puerarin, daidzein, genistein, quercetin, irisolidone, biochanin A, biochanin B, isoorientin and mangiferin, through which it exerts its beneficial activities mainly anti-inflammatory, antioxidant, antistress, nootropic, hypolipidemic, cardioprotective, among others.28 The anti-inflammatory effect of extracts derived from P. tuberosa have also been attributed to the enhanced activity of the antioxidant enzymes present in RBCs, which act as the second-line of defense against oxidative stress. Glutathione is the first-line of defense against the damaging effects of oxidative stress. It effectively counteracts the harmful free radicals (FRs) directly and also in collaboration with other antioxidants like vitamins E and C.29
CONCLUSION
The results of the present clinical study demonstrated that “Sangfer” is highly effective for the treatment of anemia during pregnancy, as evidenced by the significant increase in the blood hemoglobin level, anemia sign and symptoms and PGA scores. Furthermore, during the 84-day treatment period, no significant changes in vital signs were observed. There were no treatment-related side effects reported by any of the study participants.
REFERENCES
- Sirdah MM, Yaghi A, Yaghi AR. Iron deficiency anemia among kindergarten children living in the marginalized areas of Gaza Strip, Palestine. Rev Bras Hematol Hemoter. 2014;36(2):132-8.
- Goldenberg RL, Culhane JF. Low birth weight in the United States. Am J Clin Nutr. 2007;85(2):584S-90S.
- Abu-Ouf NM, Jan MM. The impact of maternal iron deficiency and iron deficiency anemia on child’s health. Saudi Med J. 2015;36(2):146-9.
- Lee KA, Zaffke ME, Baratte-Beebe K. Restless legs syndrome and sleep disturbance during pregnancy: the role of folate and iron. J Womens Health Gend Based Med. 2004;10(4):335-41.
- Milman N. Postpartum anemia II: prevention and treatment. Ann Hematol. 2012;91(2):143-54.
- Beard J. Iron deficiency alters brain development and functioning. J Nutr. 2003;133(5 Suppl 1):1468S-72S.
- Shill KB, Karmakar P, Kibria G, Das A, Rahman MA, Hossain MS, et al. Prevalence of iron-deficiency anaemia among university students in Noakhali region, Bangladesh. J Health Popul Nutr. 2014;32(1):103-10.
- Zimmerman MB, Hurrell RF. Nutritional iron deficiency. Lancet. 2007;370(9586):511-20.
- Schaefer RM, Huch R, Krafft A; Anaemia Working Group. Current recommendations for the treatment of iron deficiency anemia. Rev Med Suisse. 2007;3(105):874-80.
- Khandelwal DA, Donga SB, Dei L. Clinical efficacy of Punarnava Mandura and Dhatri Lauha in the management of Garbhini Pandu (anemia in pregnancy). Ayu. 2015;36(4):397-403.
- Choudhary B, Shetty A, Langade DG. Efficacy of Ashwagandha (Withania somnifera [L.] Dunal) in improving cardiorespiratory endurance in healthy athletic adults. Ayu. 2015;36(1):63-8.
- Kulkarni SK, Dhir A. Withania somnifera: an Indian ginseng. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(5):1093-105.
- Gupta GL, Rana AC. Withania somnifera (Ashwagandha): a review. Pharmacogn Rev. 2007;1(1):129-36.
- Borichangar R, Kalavadiya K, Shukla K, Jain S. Evaluation of anti-anemic activity of Withania somanifera root extract in quinidine induced anemia in rats. IJCRT. 2020;8(10):3507-13.
- Ziauddin M, Phansalkar N, Patki P, Diwanay S, Patwardhan B. Studies on the immunomodulatory effects of Ashwagandha. J Ethnopharmacol. 1996;50(2):69-76.
- Venkatasubramanian P, Koul IB, Varghese RK, Koyala S, Shivakumar A. Amla (Phyllanthus emblica) enhances iron dialysability and uptake in in vitro models. Curr Sci. 2014;107(11):1859-66.
- Variya BC, Bakrania AK, Patel SS. Emblica officinalis (Amla): a review for its phytochemistry, ethnomedicinal uses and medicinal potentials with respect to molecular mechanisms. Pharmacol Res. 2016;111:180-200.
- Mishra V, Puranik V, Singh V, Verma M, Yadav N, Rai GK. Development of vitamin C rich value added beverage. Am J Food Technol. 2012;7:222-9.
- Khan KH. Roles of Emblica officinalis in medicine - a review. Bot Res Intl. 2009;2(4):218-28.
- Akter T, Akhter QS, Amran MdS, Lisa SH, Sultana A, Sultana F, et al. Haematopoietic effects of Amloki (Emblica officinalis) in pregnancy with iron deficiency anaemia. J Biosci Med. 2020;8:157-65.
- Sharp P, Srai SK. Molecular mechanisms involved in intestinal iron absorption. World J Gastroenterol. 2007;13(35):4716-24.
- Sana H, Sinha MP. Effect of Emblica officinalis fruit extracts on haematological profile and serum lipid variables of albino rats. Glob J Pharm. 2015;9(4):311-5.
- Attar U, Banger R, Avhad P. Review on Shatavari. IJNRD. 2023;8(1):d29-37.
- Velavan S, Nagulendran KR, Mahesh R, Begum VH. The chemistry, pharmacological and therapeutic applications of Asparagus racemosus: a review. Phcog Rev. 2007;1(2):350-60.
- Chaudhary B, Jyothi Y, Rabbani SI. Potential effect of Asparagus racemosus root extract on experimental anemic and thrombocytopenic conditions in rats. J Pharm Res. 2016;15(1):15-9.
- Shukla R, Banerjee S, Tripathi YB. Antioxidant and antiapoptotic effect of aqueous extract of Pueraria tuberosa (Roxb. Ex Willd.) DC. On streptozotocin-induced diabetic nephropathy in rats. BMC Complement Altern Med. 2018;18(1):156.
- Babu PV, Bandi S, Raju MG, Prathima M, Tiwari VK. Antioxidant and immunosuppressant activity of Pueraria tuberosa. IJPPR Hum J. 2016;8(1):23-34.
- Bharti R, Chopra BS, Raut S, Khatri N. Pueraria tuberosa: a review on traditional uses, pharmacology, and phytochemistry. Front Pharmacol. 2021;11:582506.
- Pandey N, Yadav D, Pandey V, Tripathi YB. Anti-inflammatory effect of Pueraria tuberosa extracts through improvement in activity of red blood cell anti-oxidant enzymes. Ayu. 2013;34(3):297-301.