https://doi.org/10.59793/ijcp.v34i8.761
Abstract
Scrub typhus, also known as Bush typhus, is a zoonotic infectious disease predominantly affecting rural and semi urban areas. It is caused by the bacterium Orientia tsutsugamushi. Scrub typhus is predominantly seen in monsoon and post-monsoon seasons. It a vector-borne disease and has a varying clinical presentation ranging from mild acute febrile illness to life-threatening multiorgan dysfunction. Neurological manifestations can occur in the form of meningitis, meningoencephalitis, polyneuritis cranialis, intracerebral hemorrhage; rarely, it can cause cerebellar dysfunction. Herein, we report a case of acute bilateral cerebellar ataxia, one of the rare neurological complications of scrub typhus.
Keywords: Bush typhus, zoonotic, Rickettsia, neurological complications
Scrub typhus is a common zoonotic disease, which is endemic in the Asia-Pacific region. Cases are usually on the rise during monsoon and post-monsoon season. It is caused by an intracellular Gram-negative organism Orientia tsutsugamushi (formerly called Rickettsia tsutsugamushi), belonging to the Rickettsiaceae family.1 Scrub typhus is a vector-borne disease, which is transmitted to humans via an arthropod vector of the Trombiculidae family. Mite can serve as both vector and reservoir. Scrub typhus can affect people of all the ages and is a serious public health problem in countries with high prevalence. Although this disease is seen worldwide, it is endemic to a part of world known as the “tsutsugamushi triangle”, which extends from northern Japan and eastern Russia in the north to northern Australia in the south and to Pakistan and Afghanistan in the west.2-4
The incubation period of scrub typhus is 6 to 21 days. The onset is characterized by fever, myalgia, headache, cough and gastrointestinal symptoms like nausea and vomiting. A classical case may have black eschar at the site of chigger bite and it can be present at any body part. But this is seen only in very few cases. Patient may develop regional or generalized lymphadenopathy with enlarged and tender lymph nodes. If untreated, patient may develop complications like acute respiratory distress syndrome (ARDS) with lung infiltrates, renal failure, pancreatitis, thrombocytopenia with bleeding manifestations, myocarditis and pan-digital gangrene. The clinical presentation therefore may vary from a mild disease to severe multiorgan dysfunction with high case fatality rates.
Common neurological complications of scrub typhus include state of altered sensorium, aseptic meningitis, seizure, meningoencephalitis. But some rare manifestations include pan-digital gangrene,4 cerebrovascular accident (CVA),5 acute disseminated encephalomyelitis (ADEM), cerebellar dysfunction, multiple cranial nerve palsies6,7 and disseminated intravascular coagulation (DIC). Acute cerebellar ataxia is a rare complication of scrub typhus, which was seen in our patient.
CASE REPORT
A 21-year-old married, housewife female was admitted to Female Medicine Ward of RNT Medical College, Udaipur, Rajasthan with complaints of high-grade fever with chills for 15 days, nausea/vomiting for 12 days, altered sensorium and headache for 2 days. There was no history of seizure/dyspnea. She had been treated with antimalarials, antibiotics, antipyretics and intravenous fluids but the symptoms did not subside and instead she developed complications for which she was brought to our hospital. At the time of admission, patient was in a state of altered sensorium, irritable and not oriented to time, place and person. Her vital signs were pulse 120/min, respiratory rate 22/min, oxygen saturation (SpO2) was 97% at room air and temperature was 102oF (axilla). Her general physical examination revealed mild pallor. No eschar, icterus, lymphadenopathy, petechiae/purpura were seen. Detailed central nervous system (CNS) examination could not be possible because patient was in altered mental state (Glasgow Coma Scale [GCS] = E2V2M5) and irritable but there were no signs of meningeal irritation; pupils were bilaterally symmetrical and reactive to light and the plantar response was bilaterally mute. Other systemic examination (respiratory/cardiovascular/gastrointestinal) showed no abnormality. So, a clinical diagnosis of acute febrile illness, i.e., cerebral malaria, scrub meningoencephalitis, meningitis and viral encephalitis was made.
Comprehensive laboratory investigations were performed. The complete blood count (CBC) showed hemoglobin - 11 g/dL, total leukocyte count (TLC) - 9,200/cu mm, platelet count - 2.35 lakhs/cu mm. The liver and kidney function tests (LFT/KFT), chest X-ray, ECG, noncontrast CT (NCCT) scan of the head were unremarkable. Viral markers for hepatitis B and C viruses and human immunodeficiency virus (HIV) were also negative. Examination of cerebrospinal fluid (CSF) showed total protein - 184 mg/dL, total cells - 178/cu mm (90% - lymphocytes, 10% other mononuclear cells).
This patient was further subjected to specific tests relevant to acute febrile illness like CSF-adenosine deaminase (ADA) and CSF cartridge-based nucleic acid amplification test (CB-NAAT) for Mycobacterium tuberculosis along with CSF polymerase chain reaction (PCR) neuro-panel (for human adenovirus, enterovirus, parechovirus, HSV-1 and 2, parvovirus B19, Epstein-Barr virus, varicella-zoster virus, cytomegalovirus, herpes virus 6 and 7), which were negative. Dengue virus NS1 antigen, Dengue IgM (by ELISA), malaria parasite quantitative buffy coat (MP-QBC), serum ELISA test for chikungunya, Rubella, Japanese encephalitis viruses were also negative. Scrub typhus IgM (by ELISA) came positive. Ultrasonography of whole abdomen revealed altered echo texture of liver.
A diagnosis of scrub meningoencephalitis was made and patient was put on injection doxycycline 100 mg IV twice-daily and injection chloramphenicol 1 g IV thrice-daily along with symptomatic treatment with hydration, antipyretics and supportive care. Magnetic resonance imaging (MRI) brain (contrast-enhanced) was planned, which revealed T2/FLAIR hyperintensity in bilateral cerebellum without diffusion restriction on DWI (suggestive of cerebellitis) (Fig. 1). The patient subsequently become afebrile 3 to 4 days after treatment and started following commands. During her recovery phase, examination of the nervous system revealed dysarthric, staccato and scanning speech, head titubation, bilateral upper and lower limb in coordination in form of abnormal finger-nose and heel-shin-knee test, abnormal rapid alternating movements, wide based gait with cerebellar ataxia, truncal ataxia, nystagmus and tremors of both hands. Cranial nerve/motor/sensory examinations were within normal limits. During hospital stay, the patient was shifted to oral doxycycline and chloramphenicol. She was discharged on doxycycline and chloramphenicol for 14 days and instructed to visit Medicine OPD for follow-up.
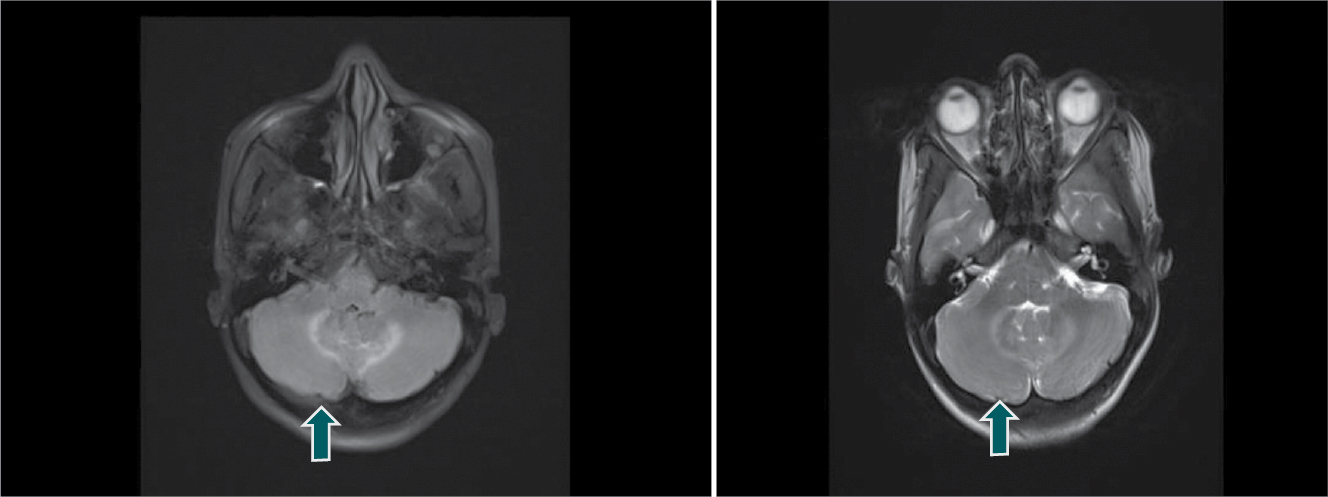
Figure 1. Contrast-enhanced MRI brain showing bilateral cerebellar hyperintensities (arrows) on T2 FLAIR (left) and T2 images (right) suggestive of bilateral cerebellitis.
DISCUSSION
Scrub typhus is a zoonotic disease, which has re-emerged in various part of India in last few years including southern Rajasthan. It shows seasonal variation; hence cases are predominantly seen during monsoon and post-monsoon season (i.e., July to November). It is transmitted by the bite of the chigger larvae of trombiculid mite. Man is an accidental host. Infection rates are higher in people living in rural areas with habit of open defecation, bare foot walking, people engaged in farming.8
The clinical manifestation can vary from mild acute febrile illness to severe illness mainly in untreated cases, which can even progress to various neurological complications and multiorgan dysfunction. The common neurological complications are aseptic meningitis, meningoencephalitis, and rare ones include cerebellitis, cerebral hemorrhage, ADEM, myelitis, cerebral infarction. As in our case report, the patient presents with isolated cerebellitis.
Previously Gupta et al7 and Mahajan et al8 have also reported isolated cerebellitis as a complication of scrub typhus. The likely pathophysiology is microangiopathy leading to focal or disseminated vasculitis or perivasculitis.9-11
Acute cerebellitis is a state of acute cerebellar dysfunction in which patient presents with incoordination, imbalance, gait instability, speech abnormality. Possible etiologies are viral and post viral infections, as part of disseminated meningoencephalitis, infarction or hemorrhage within cerebellar hemisphere, drugs and toxin (phenytoin, carbamazepine, lithium), inherited cerebellar ataxia like spinocerebellar ataxia (SCA), tumors. Scrub typhus rarely can cause bilateral cerebellitis as in our case. Other possible causes for acute cerebellitis should be ruled out. MRI may or may not be normal.7,12
Our case showed T2/FLAIR hyperintensity involving bilateral cerebellum. Scrub typhus response to doxycycline treatment is dramatic. Our patient too improved within 3 to 4 days of starting treatment for scrub typhus. Thus, early diagnosis and treatment is crucial to reduce complication rate and also case fatality rates. The patient may have a favorable outcome with no or minimal neurological deficit.
CONCLUSION
Scrub typhus is a growing or emerging disease in various parts of world and the Indian subcontinent. Case fatality rates in untreated cases are 7% but it can be as high as 30%. It can be missed because of the various atypical presentations; hence, high index of suspicion is required with knowledge of various common and uncommon complications. Early diagnosis and prompt treatment definitely results in better outcome. The purpose of this case report was to increase awareness about this rare presentation of scrub typhus.
REFERENCES
- Scrub typhus. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/typhus/scrub/index.html.
- Rapsang AG, Bhattacharyya P. Scrub typhus. Indian J Anaesth. 2013;57(2):127-34.
- Dave MK, Sareen M, Vignesh A. Epidemiology, clinical presentation, lab diagnosis and outcome of scrub typhus outbreak in a tertiary care center in Southern Rajasthan. J Assoc Physicians India. 2022;70(4):11-2.
- Dave M, Jain S, Nath H, Nagraj. Digital gangrene: a rare complication in scrub typhus. JIACM. 2020;21(3-4):187-9.
- Dave M, Saini HL, Jain S, Nyati A, Patel P. Scrub typhus with cerebrovascular accident (intracerebral haemorrhage): a rare case presentation. RUHS J Health Sci. 2020;5(3):176-8.
- Shetty VN, Rao G, Jayaprakash B. An atypical presentation of scrub typhus. Int J Adv Med. 2022;9(10):1069-71.
- Gupta S, Grover S, Gupta M, Kaur D. Cerebellitis as a rare manifestation of scrub typhus fever. BMJ Case Rep. 2020;13(5):e233993.
- Mahajan SK, Sharma S, Kaushik M, Raina R, Thakur P, Taneja GP, et al. Scrub typhus presenting as acute cerebellitis. J Assoc Physicians India. 2016;64(2):69-70.
- Hornick RB. Goldman: Cecil Textbook of Medicine. In: Bennett JC, Plum F (Eds.). Philadelphia, USA: WB Saunders Company; 2000.
- Saxena A, Khiangte B, Tiewsoh I. Scrub typhus complicated by acute respiratory distress syndrome and multiorgan failure; an unrecognized alarming entity in central India: a report of two cases. J Family Med Prim Care. 2014;3(1):80-3.
- Ono Y, Ikegami Y, Tasaki K, Abe M, Tase C. Case of scrub typhus complicated by severe disseminated intravascular coagulation and death. Emerg Med Australas. 2012;24(5):577-80.
- Bhoil R, Kumar S, Sood RG, Bhoil S, Verma R, Thakur R. Cerebellitis as an atypical manifestation of scrub typhus. Neurology. 2016;86(22):2113-4.