Abstract
Kikuchi-Fujimoto disease (KFD), also known as histiocytic necrotizing lymphadenitis, is a rare condition of unknown etiology presenting with cervical lymphadenopathy along with associated symptoms of fever, weight loss. It is often misdiagnosed due to rare existence. We report a case of a 21-year-old female who presented with painful cervical lymphadenopathy and low-grade fever on and off for 6 months. Examination revealed left-sided multiple, tender, matted lymph nodes measuring maximum 2 cm in size, firm and mobile. Patient underwent a panel of investigations including cervical biopsy, which revealed findings of KFD.
Keywords: Kikuchi-Fujimoto disease, recurrent histiocytic necrotizing lymphadenitis, systemic lupus erythematosus
Kikuchi-Fujimoto disease (KFD) is a rare form of painful lymphadenopathy, which is more common in Southeast Asia. KFD is not very well described in Africa, with very few reports described in the literature. The lymphadenopathy is usually cervical with associated nonspecific symptoms of fever and night sweats, which makes the diagnosis more challenging as the differential diagnosis is wide.1 We describe the case of a young female, who presented with painful multiple cervical lymphadenopathy in cervical region and later confirmed to have KFD on lymph node biopsy.
CASE PRESENTATION
A 21-year-old female presented with features of multiple, tender, soft to firm, mobile, nonadherent to adjacent tissue, matted, left cervical lymph node enlargement for about 6 months duration, and associated low-grade fever off and on. There was no history of weight loss, night sweats, cough, breathlessness, any swellings in other sites, generalized weakness and fatigue, butterfly rash, photosensitivity, oral ulcers, hair loss, palpitations, heat intolerance or dry mouth. Examination revealed enlarged lymph nodes in the left cervical region measuring maximum 2 cm in size, firm and mobile. There was no pallor, icterus, and clubbing.
Respiratory system examination revealed no abnormality and on per abdomen examination no hepatosplenomegaly was found. Patient underwent a panel of investigations including complete blood count (CBC) with peripheral smear, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR) and thyroid profile. Mantoux test was found to be indeterminate. Urine routine was normal, and microscopy showed no sediments.
Ultrasonography (USG) of abdomen did not show any lymphadenopathy. USG left cervical region showed few enlarged level V cervical lymph nodes. Patient underwent cervical lymph node biopsy, which revealed histiocytic necrotizing lymphadenitis suggestive of KFD (Figs. 1 and 2).

Figure 1. Profile picture of patient showing scar mark on lateral side of neck (post-excisional).
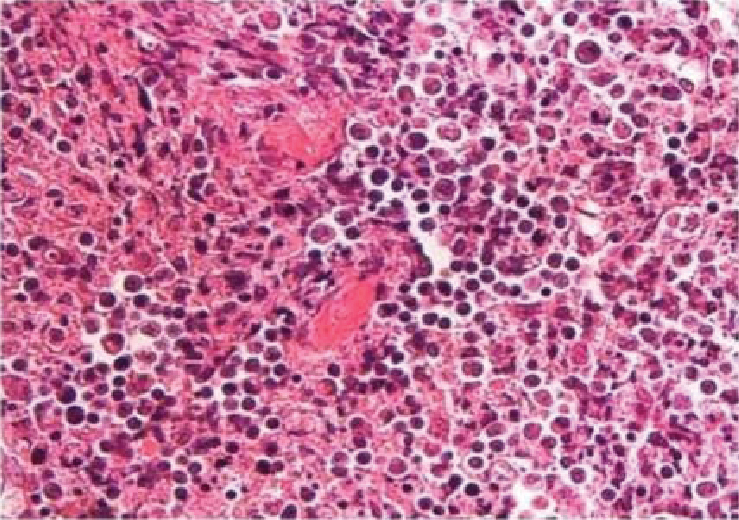
Figure 2. Lymph node biopsy showing numerous foci of necrosis with apoptotic bodies and scattered histiocytes. Absence of acute inflammatory infiltrate and hematoxylin bodies are suggestive of Kikuchi’s disease.
On detailed history, it was found that patient had a similar complaint 1.5 years ago for which she underwent excisional biopsy that showed KFD and the patient was treated for it. The disease subsided after treatment with complete regression of lymph nodes. We report this case of relapse of KFD, as there are very few reports of relapse (3%) making it rare.
Patient was started on nonsteroidal anti-inflammatory drugs (NSAIDs) along with oral corticosteroids, hydroxychloroquine and leflunomide with symptomatic improvement.
DISCUSSION
Kikuchi-Fujimoto disease, also known as histiocytic necrotizing lymphadenitis, is commonly seen in females of 20 to 30 years age group with self-limiting lymphadenopathy (disappears within 1 to 4 months)2. A low but possible recurrence rate of 3% to 4% has been seen. Recurrence has been recorded over a period of 2 to 10 years after the initial presentation3. Our case represents a shorter recurrence course (within 1.5 years). The exact pathophysiology of KFD is not known, and postulated theories are of infectious and autoimmune origins. KFD is commonly found in association with systemic lupus erythematosus (SLE)4, Still’s disease, Grave’s disease and Sjogren’s disease. Clinical features include lymphadenopathy, fever, fatigue, joint pain, high ESR, CRP and erythematous rashes. Cervical region is the commonest site for lymphadenopathy and is usually painful3,5.
The clinical picture is often nonspecific and should be differentiated from tuberculosis (TB)2,4, infectious mononucleosis, lymphoma, and metastatic cancer. Due to the frequent association with SLE (30%)4, regular follow-ups and screening for diagnosis of SLE is recommended. The diagnosis is confirmed on histopathology showing architecture of follicular hyperplasia and necrotic abundant karyorrhectic nucleardebris. Histiocytes are positive for lysozyme, myeloperoxidase, CD68, CD163, and CD4 cells.
Patients with mild disease respond to supportive care with antipyretics and NSAIDs1,6. Treatment options for aggressive and recurrence cases include use of corticosteroids and immunosuppressors3. Symptomatic treatment is the main medical intervention but there are documented cases of recurrence, who need treatment with corticosteroids and other immunosuppressant drugs.
CONCLUSION
Kikuchi’s disease can present with infective lymphadenopathy and therefore should be considered in the differential diagnoses of enlarged lymph nodes. Histological examination is the gold standard to diagnose the condition and to avoid unnecessary treatment. Usually, complete regression of disease occurs, but it can rarely recur in 3% cases. A high degree of clinical suspicion is required to make the diagnosis and detailed history with lymph node biopsy reports should not be missed out.
REFERENCES
- Sharma K, Otieno F, Shah R. Case report of Kikuchi-Fujimoto disease from Sub-Saharan Africa: an important mimic of tuberculous lymphadenitis. Case Rep Med. 2020;2020:4385286.
- Dhukiya R. Kikuchi’s disease: a case report from west India. Int J Allied Med Sci Clin Res. 2020;2(4):322-5.
- Singhania P, Paul R, Maitra S, Banerjee A, Hashmi M. Kikuchi-Fujimoto disease from eastern India. J Glob Infect Dis. 2010;2(3):305-6.
- Achappa B, Herath NC, Sebastian B, Dsouza NV, Raghuram PM, Holla R, et al. Kikuchi- Fujimoto disease in a tertiary care teaching hospital in Coastal South India: a 8-year retrospective study. F1000Res. 2022;11:492.
- Pai VD, Jadhav RR. Kikuchi’s disease: a diagnostic dilemma. Indian J Surg. 2015;77(Suppl 1):164-5.
- Wilson MR, Milne G, Vryonis E. Kikuchi-Fujimoto disease: a rare cause of fever in the returning traveler. Case Rep Med. 2014;2014:868190.