Abstract
Hypoxemic respiratory failure is a rare presentation of active pulmonary tuberculosis (TB). Though tuberculous acute respiratory distress syndrome (ARDS) is well documented in medical literature, non-ARDS respiratory failure is seldom reported in active pulmonary TB. We herein report a case, which posed a diagnostic dilemma as it clinically mimicked interstitial lung disease. Imaging showed unilateral localized smooth interlobular septal thickening along with consolidation without significant mediastinal lymphadenopathy. To the best of our knowledge, this rare radiological finding has not been reported in medical literature as being associated with hypoxemic respiratory failure in pulmonary TB patients.
Keywords: Pulmonary TB, TB, hypoxemic respiratory failure, interlobular septal thickening
Pulmonary tuberculosis (TB) has been recognized as a scourge of humanity since antiquity. The disease continues to ravage much of the developing world and is still the most common infection causing death. One-fourth of the world population is estimated to be infected with Mycobacterium tuberculosis, although the distribution is heterogeneous1. TB has a myriad of clinical presentations making its diagnosis challenging.
Here we present a rare case of a patient who presented with type 1 respiratory failure and was clinically suspected to have interstitial lung disease but got microbiologically diagnosed with pulmonary TB and improved with antitubercular medications. This case report emphasizes the importance of a high degree of clinical suspicion for pulmonary TB in endemic countries like India.
CASE REPORT
A 74-year-old male farmer with a history of working in a cotton mill for 12 years, never-smoker, presented with complaints of breathlessness on exertion for the last 4 months. The breathlessness was insidious in onset and progressed from Grade 0 on the Modified Medical Research Council (mMRC) dyspnea scale to Grade IV. He gave a history of dry cough for the past 10 years with no diurnal, seasonal or postural variation. There was no history of fever, hemoptysis, weight loss, wheezing, chest tightness, joint pains, rash or Raynaud’s syndrome. He had no other medical comorbidities or history of previous TB or severe coronavirus disease 2019 (COVID-19) infection. On evaluation, he was found to have tachycardia (heart rate - 110/min), tachypnea (respiratory rate - 35/min), hypoxemia (oxygen saturation of 72% at room air); the blood pressure was 136/84 mmHg. The patient had pallor with no evidence of clubbing, icterus or peripheral lymphadenopathy.
On auscultation, there were fine end-inspiratory crackles in bilateral lower lung zones with a predominance in the left lower regions of the chest. Arterial blood gas evaluation revealed respiratory alkalosis along with moderate hypoxemia (pH - 7.479, pCO2 - 26.9 mmHg, pO2 - 52.9 mmHg, HCO3 - 24 mmol/L and lactate - 1.2 mmol/L). He was given supplemental oxygen through a face mask at 10 L/min.
On further evaluation, he had a hemoglobin level of 9.9 g/dL, total leukocyte count of 10,500 cells/µL with a differential cell count showing 87% neutrophil, 7% lymphocytes, 3% eosinophils, 3% monocytes and platelets of 1.53 lakh/cu mm. Serum biochemistry revealed urea - 41 mg/dL, creatinine - 0.81 mg/dL, aspartate aminotransferase (AST) - 103 IU/L, alanine aminotransferase (ALT) - 85 IU/L, sodium - 130 mEq/L, potassium - 4.3 mEq/L, total protein - 6.4 g/dL and albumin - 2.1 g/dL.
Chest radiography demonstrated a hyperinflated lung field with reticular opacities in the right upper zone, left upper and middle zones with nonhomogenous air space opacities and features of volume loss in the form of rib crowding in the left upper and middle zone (Fig. 1).

Figure 1. Chest radiography (PA view) demonstrating a hyperinflated lung field with reticular opacities in the right upper zone, left upper and middle zone. Left upper and middle zone shows rib crowding along with nonhomogenous air space opacities.
Gram stain and Ziehl-Neelsen (ZN) stain done on induced sputum were negative. The viral markers for human immunodeficiency virus (HIV) and hepatitis B virus (HBV) were negative. High-resolution computed tomography (HRCT) of the chest taken for further evaluation of the patient revealed bilateral apical emphysematous changes with interlobular septal thickening in the left lingula and left lower lobe with consolidation in the left lower lobe with no significant mediastinal lymphadenopathy (Fig. 2).
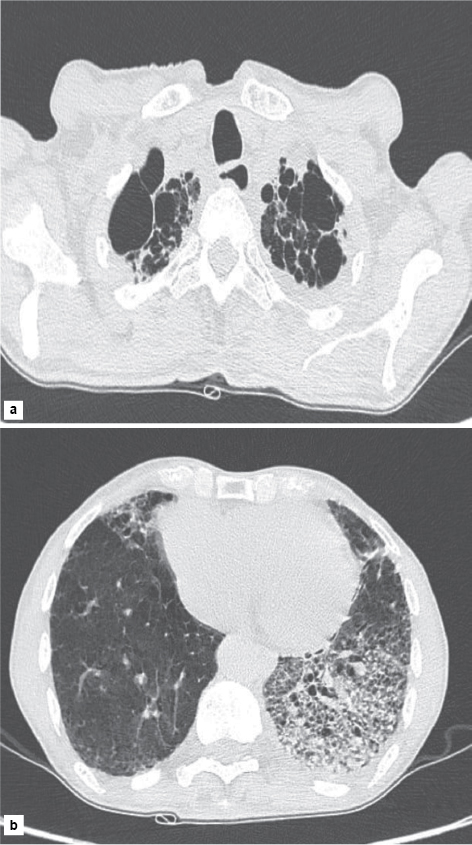
Figure 2. HRCT of the chest demonstrating (a) bilateral apical emphysematous changes (b) interlobular septal thickening in the left lingula and left lower lobe with consolidation in the left lower lobe.
He underwent videobronchoscopy and bronchoalveolar lavage (BAL) was taken from the left lower lobe superior segment. Cartridge-based nucleic acid amplification test (CB-NAAT) done on BAL revealed high levels of M. tuberculosis with no rifampicin resistance. BAL Gram stain and ZN stain were negative.
He was diagnosed with microbiologically-confirmed pulmonary TB and was put on first-line antitubercular drugs. He responded well to treatment and was weaned off supplemental oxygen after 6 weeks of starting antitubercular therapy.
DISCUSSION
India bears the highest burden of TB with an incidence of 210 per 1,00,000 population in 20212. Acute hypoxemic respiratory failure is a rare presentation of pulmonary TB with an incidence of only 1.7% and mortality nearing 53%3,4.
Our patient was clinically suspected to have acute exacerbation of interstitial lung disease as he had history of significant exposure to cotton dust, chronic dry cough with progressive dyspnea, fine crackles on auscultation and hypoxemia. He had no history of exposure to an active pulmonary TB case, no fever or significant weight loss. Chest radiography prompted us to further evaluate the patient for infective etiology of hypoxemic respiratory failure but the HRCT of the patient added to the existing diagnostic dilemma. CB-NAAT performed on the patient’s BAL was crucial in diagnosing the patient.
Even though TB ARDS has been documented in medical literature5, our patient with unilateral localized radiological lesions did not satisfy Berlin’s criteria for ARDS. Bronchogenic pulmonary TB, extensive parenchymal consolidation, bilateral smooth interlobular septal thickening and miliary TB have been reported as causes of acute respiratory failure6,7. Our patient had unilateral localized interstitial involvement in the form of interlobular septal thickening along with consolidation, which to the best of our knowledge has not been reported in medical literature as a cause of hypoxemic respiratory failure in pulmonary TB. Interlobular septal thickening demonstrates a lymphatic spread of disease, which is usually associated with enlarged regional lymph nodes. Its absence in our case makes it an extremely rare presentation.
Chronic obstructive pulmonary disease (COPD) is a known risk factor for respiratory failure in active pulmonary TB8. Our patient, even though not spirometrically diagnosed with COPD, had extensive bilateral upper lobe emphysematous changes, which might have predisposed him to develop respiratory failure. In non-miliary pulmonary TB, the most dominant mechanism causing hypoxemia is the destruction of pulmonary parenchyma caused by the inflammatory response against the bacillary antigen of M. tuberculosis9. Given the destructive inflammatory response, corticosteroids have been used along with antitubercular drugs for managing TB ARDS. Their use in pulmonary TB with non-ARDS respiratory failure is controversial. Our patient was managed with first-line antitubercular drugs and was successfully weaned off oxygen within 6 weeks of initiation of therapy.
CONCLUSION
Pulmonary TB can have a myriad of clinical presentations. The clinicians should have high suspicion, especially in endemic countries like India. Unilateral interlobular septal thickening with hypoxemic respiratory failure, though rare, is a possible presentation of pulmonary TB.
Compliance with Ethical Standards
The authors have no conflict of interest to disclose. Informed written consent of the patient was taken for the publication of his medical information.
REFERENCES
- Cohen A, Mathiasen VD, Schön T, Wejse C. The global prevalence of latent tuberculosis: a systematic review and meta-analysis. Eur Respir J. 2019;54(3):1900655.
- World Health Organization (WHO). Global Tuberculosis Report 2022. Available at: https://www.who.int/publications/i/item/9789240061729. Last accessed July 4, 2023.
- Choi D, Lee KS, Suh GY, Kim TS, Kwon OJ, Rhee CH, et al. Pulmonary tuberculosis presenting as acute respiratory failure: radiologic findings. J Comput Assist Tomogr. 1999;23(1):107-13.
- Agarwal MK, Muthuswamy PP, Banner AS, Shah RS, Addington WW. Respiratory failure in pulmonary Chest. 1977;72(5):605-9.
- Mohan A, Sharma SK, Pande JN. Acute respiratory distress syndrome (ARDS) in miliary tuberculosis: a twelve year experience. Indian J Chest Dis Allied Sci. 1996;38(3):157-62.
- Kilaru SC, Prasad S, Kilaru H, Anneela RR, Hasan A, Nandury EC. Active pulmonary tuberculosis presenting with acute respiratory failure. Respirol Case Rep. 2019;7(7):e00460.
- Akira M, Sakatani M. Clinical and high-resolution computed tomographic findings in five patients with pulmonary tuberculosis who developed respiratory failure following chemotherapy. Clin Radiol. 2001;56(7):550-5.
- Frame RN, Johnson MC, Eichenhorn MS, Bower GC, Popovich J Jr. Active tuberculosis in the medical intensive care unit: a 15-year retrospective analysis. Crit Care Med. 1987;15(11):1012-4.
- Dannenberg AM Jr. Immune mechanisms in the pathogenesis of pulmonary tuberculosis. Rev Infect Dis. 1989;11 Suppl 2:S369-78.