Introduction: Scrub typhus is a mite-borne infectious disease caused by Orientia tsutsugamushi, an obligate intracellular bacterium. The disease is of greatest public health importance in rural areas of Asia and the Western Pacific Islands. The clinical manifestations range from subclinical disease to organ failure. The chief target of organism is the vascular endothelium of various organs. There is inflammation in and around the blood vessels that causes endothelial damage resulting in vascular leakage and organ dysfunction. Case report: A 70-year-old female patient, farmer by occupation, presented to us with features of acute febrile illness and shortness of breath and was diagnosed as scrub typhus with myocarditis. She subsequently developed gangrene of right little finger. The patient was investigated for infectious and noninfectious causes of vasculitis leading to gangrene. We established that the cause for gangrene was scrub typhus as evidenced by presence of eschar and positive serology. Conclusion: We report for the first time a case of scrub typhus complicated by both myocarditis and gangrene. Both myocarditis and unidigital gangrene are unusual complications of scrub typhus. Hence, scrub typhus should be ruled out in patients who present with these complications.
Keywords: Scrub typhus, Orientia tsutsugamushi, vasculitis, eschar, myocarditis, unidigital gangrene
Scrub typhus, also known as bush typhus, is a zoonotic disease caused by the bacterium Orientia tsutsugamushi. It is an obligate, intracellular, Gram-negative coccobacilli and is transmitted to humans by an arthropod vector of Trombiculidae family.
Scrub typhus spreads to people through bite of infected chiggers (infected larval mites)1. Mites remain infected throughout different stages (egg, larva, nymph and adult) of their life cycle2. Around a billion people are at risk and nearly million cases are reported every year3. Scrub typhus was first described in China in 313 AD; it later re-emerged during the Second World War4.
Scrub typhus is seen worldwide but it is endemic to a part of world known as “Tsutsugamushi Triangle”, which extends from Japan and eastern Russia to Australia in south and to Pakistan and Afghanistan in the west5. In India, the highest numbers of cases are reported from West Bengal, Assam, Meghalaya, Rajasthan, Maharashtra, and Madhya Pradesh.
Clinically, scrub typhus varies from mild and self-limiting to fatal disease. The incubation period ranges from 6 to 21 days. The onset of the disease is characterized by fever, headache, myalgia, cough, and gastrointestinal symptoms. The classic case description includes an eschar at the site of chigger bite, regional lymphadenopathy, and maculopapular rashes.2
Severe cases typically manifest with encephalitis, meningoencephalitis, myocarditis, pericardial effusion, acute renal failure, multiorgan dysfunction, and focal or pan digital gangrene.
Focal or pan digital gangrene is one among the rare complications that may occur during the acute phase or in the recovery phase of scrub typhus caused due to focal or disseminated vasculitis or perivasculitis of digital blood vessels.5
Concomitant presentation of myocarditis with digital gangrene in scrub typhus is very rare; hence, we are reporting this case.
A 70-year-old female patient, farmer by occupation, admitted to medical ICU, Maharana Bhupal Government Hospital and RNT Medical College, Udaipur, Rajasthan with the complaint of high-grade fever and chills, generalized bodyache, nausea and vomiting, and shortness of breath for last 5 days.
On general examination, the pulse rate was 118 bpm, blood pressure (BP) was 80/60 mmHg, oxygen saturation (SpO2) was 86% on room air and 96% on 6 liters of oxygen (on the day of admission). She had pallor, icterus, and fever of 100oF orally. An eschar mark was present on the back in the region of left scapula (Fig. 1).
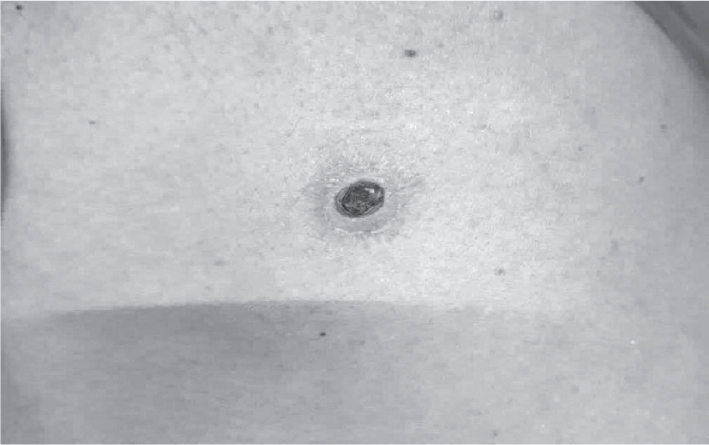
Figure 1. Showing eschar on back of chest.
On systemic examination, examination of the cardiovascular system revealed tachycardia, hypotension with muffling of heart sounds without any murmur. Other systemic examination was normal. No organomegaly in the form of hepatosplenomegaly was seen.
Clinically, we diagnosed the patient as acute fertile illness with eschar without organomegally suspected to be scrub typhus with cardiogenic shock.
Patient was investigated for acute febrile illness. Laboratory investigations showed hemoglobin (Hb) - 7.6 g/dL, total leukocyte count (TLC) - 8,400 /µL, platelet count - 58,000/µL, blood urea - 182 mg/dL, serum creatinine - 2.7 mg/dL, total bilirubin - 2.07 mg/dL, and direct bilirubin - 1.2 mg/dL.
ECG showed T wave inversion from V2 to V6 (Fig. 2). Trop T on the day of admission was 0.4. Both were monitored daily. Trop T initially increased to 0.7 on the second day. But on the fifth day, both ECG (Figs. 3 and 4) and Trop T were normal.
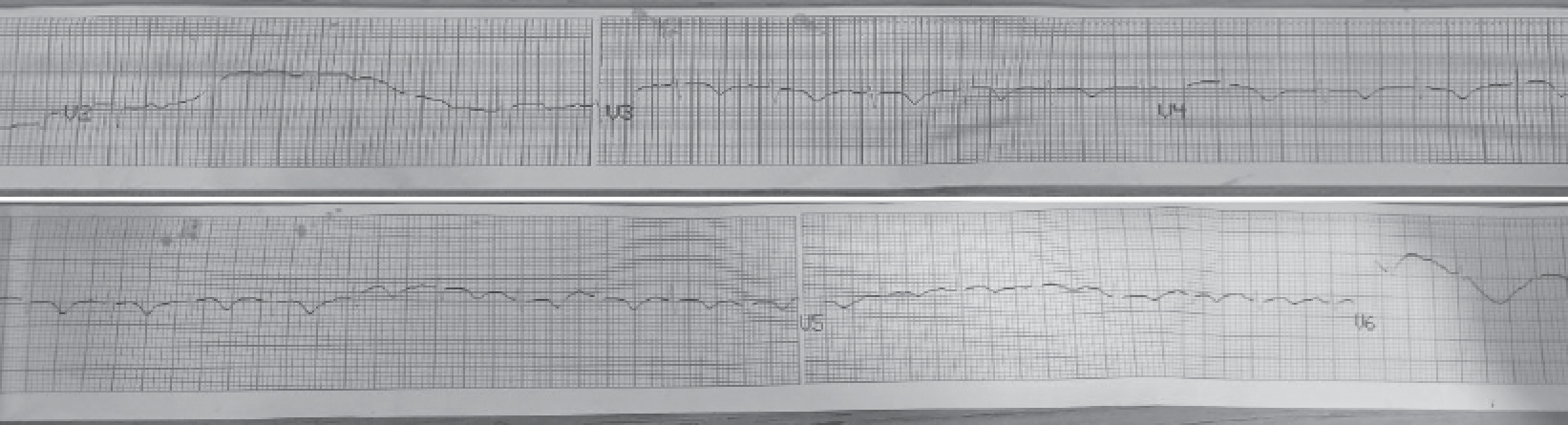
Figure 2. Showing T wave inversion from V2 to V6 (day 1).
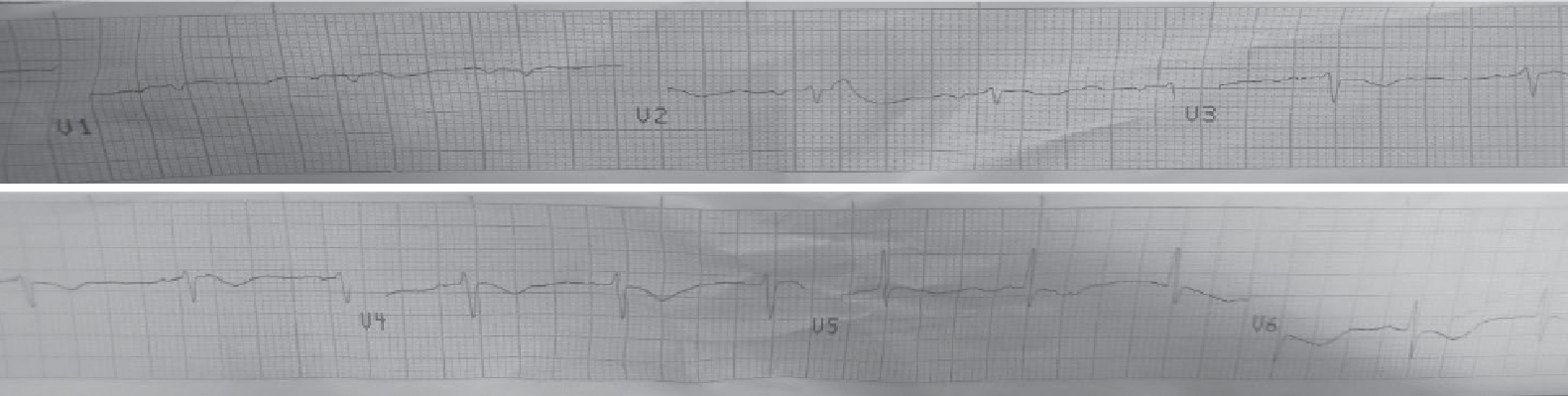
Figure 3. Showing T wave inversion reverting to normal (day 3).
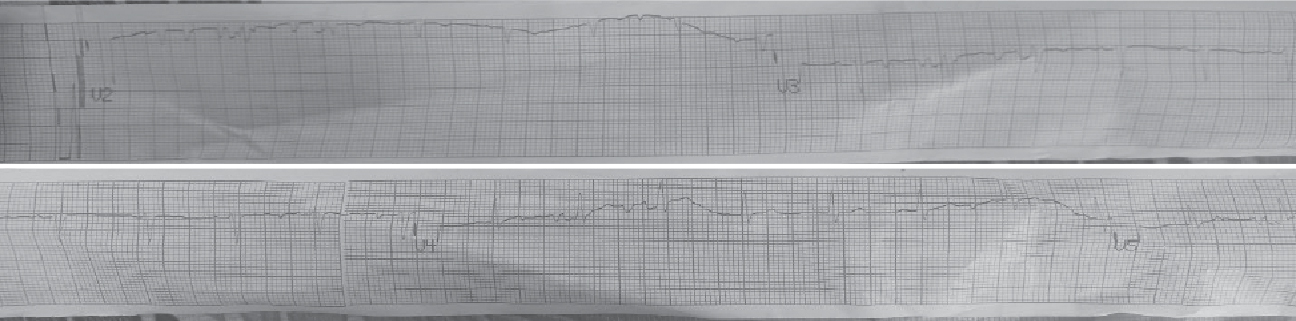
Figure 4. Showing T wave inversion reverted to normal (day 5).
Chest X-ray, ultrasound abdomen and pelvis were normal. 2D Echocardiogram showed diastolic dysfunction with mild mitral regurgitation. Human immunodeficiency virus (HIV), hepatitis B surface antigen (HBsAg) and hepatitis C virus antibodies (anti-HCV), venereal disease research laboratory (VDRL) tests were negative. Urine analysis was normal.
Specific investigations for acute febrile illness were performed. Dengue IgM, IgG antibodies and NS1 antigen were negative.
Blood smear and quantitative buffy coat test for malaria parasite were negative. But IgM ELISA (enzyme-linked immunosorbent assay) for scrub typhus was positive. Hence, etiological diagnosis of scrub typhus with myocarditis with multiorgan dysfunction was made.
Patient was put on symptomatic management with antibiotics (doxycycline 100 twice daily), antimalarial drugs, antipyretics, intravenous (IV) fluids and inotrope support.
Despite treatment, the patient complained of burning sensation and blackish discoloration of fingers of the right hand. On examination, we found dry gangrene of the little finger and blackish discoloration of other fingers with a line of demarcation (Fig. 5); peripheral pulses were normal. The patient was referred to a cardiothoracic surgeon, who advised color Doppler of arteries of all four limbs and to also rule out other causes of gangrene such as infectious and autoimmune diseases. HIV, HBsAg, VDRL were nonreactive; the antinuclear antibody (ANA), anti-double stranded DNA (anti-dsDNA), lupus erythematosus cell, cytoplasmic antineutrophil cytoplasmic antibody (c-ANCA), perinuclear anti-neutrophil cytoplasmic antibodies (p-ANCA) tests were also negative. Color Doppler of arteries of all four limbs was normal. Hence, we concluded that scrub typhus was the cause for gangrene.

Figure 5. Showing dry gangrene of little finger.
The patient was treated with antiplatelets, anticoagulants and steroids. When the patient improved clinically, the ionotrope support was tapered and stopped. The patient was discharged and asked to come for review in Medicine as well as Cardiothoracic Vascular Surgery (CTVS) OPDs.
Scrub typhus is a serious public health problem of Asia-Pacific region. With involvement of multiple organs, serious complications may develop, which could make the disease potentially fatal.
Myocarditis can be a clinical manifestation of scrub typhus but has rarely been reported. It is usually subclinical and therefore ignored many times6. Patient may present with chest pain, shortness of breath, palpitation, cardiogenic shock, congestive heart failure, ECG changes of myocarditis and elevated cardiac enzymes.
Digital gangrene is sign of systemic disease, which can be seen in infectious diseases such as syphilis, leprosy, viral hepatitis, HIV meningococcemia, leptospirosis, and other noninfectious diseases like autoimmune disease such as polyarteritis nodosa, Wegener’s granulomatosis (now called granulomatosis with polyangiitis), Churg-Strauss syndrome (involvement of medium-sized artery and systemic lupus erythematosus [SLE]), rheumatoid arthritis, scleroderma, and antiphospholipid syndrome, which may commonly involve small vessels and present with digital gangrene7.
Gangrene is an uncommon complication of rickettsial disease and very few cases have seen reported worldwide yet. The distribution of gangrene may be due to selective proliferation of these bacteria in cooler body regions leading to vasculitis, perivasculitis, tissue hypoperfusion and gangrene development8.
Rijhwani et al9 reported pan-digital gangrene in scrub typhus as a rare case. Avasthi et al10 reported acute fulminant myocarditis in scrub typhus as a rare case. Bharathi et al11 also reported similar cases. But to the best of our knowledge, no case reports have been found on scrub typhus complicated by both myocarditis and digital gangrene in the same patient.
Scrub typhus is a re-emerging zoonotic disease in the Indian subcontinent. It is a multiorgan disease as it involves endothelial dysfunction of small blood vessels. Vasculitis is among the serious complications of scrub typhus, which can lead to digital ischemia, gangrene, and myocarditis.
Proper evaluation and early diagnosis and treatment with doxycycline and steroids can help to prevent the development of complications. Our patient showed improvement in the form of disappearance of discoloration of other fingers of right hand at the time of discharge. While going through literature, we found out that a case of concomitant myocarditis and unidigital gangrene in scrub typhus had not yet been reported.
- Traub R, Wisseman CL Jr. The ecology of chigger-borne rickettsiosis (scrub typhus). J Med Entomol. 1974;11(3):237-303.
- Luce-Fedrow A, Lehman ML, Kelly DJ, Mullins K, Maina AN, Stewart RL, et al. A review of scrub typhus (Orientia tsutsugamushi and related organisms): then, now, and tomorrow. Trop Med Infect Dis. 2018;3(1):8.
- Watt G, Parola P. Scrub typhus and tropical rickettsioses. Curr Opin Infect Dis. 2003;16(5):429-36.
- Scrub typhus. Dated September 29, 2023. Available at: https://emedicine.medscape.com/article/971797-overview#a1. Accessed October 2, 2023.
- Dave M, Jain S, Nath H, Nagraj. Digital gangrene: a rare complication in scrub typhus. JIACM. 2020;21(3-4):187-9.
- Soerjomataram I, Bray F. Planning for tomorrow: global cancer incidence and the role of prevention 2020–2070. Nat Rev Clin Oncol. 2021;18(10):663-72.
- Cracco C, Delafosse C, Baril L, Lefort Y, Morelot C, Derenne JP, et al. Multiple organ failure complicating probable scrub typhus. Clin Infect Dis. 2000;31(1):191-2.
- Premaratna R, Chandrasena TG, Dassayake AS, Loftis AD, Dasch GA, de Silva HJ. Acute hearing loss due to scrub typhus: a forgotten complication of a reemerging disease. Clin Infect Dis. 2006;42(1):e6-8.
- Rijhwani P, Charan A, Agrawal CM, Pahadia MR, Gupta S, Anand H. Pan digital gangrene: a rare phenomenon in scrub typhus. J Mahatma Gandhi Univ Med Sci Tech. 2017;2(1):35-7.
- Avasthi GI, Patel P, Kuka R, Mahajan R. Acute fulminant myocarditis as a rare manifestation in complicated scrub typhus: a case report. IHJ Cardiovasc Case Rep. 2018;2(Suppl):S18-S20.
- Bharathi SL, Jayachandran S, Senthil N, Sujatha S. Scrub typhus causing myocarditis and ARDS: a case report. Heart India. 2013;1(3):85-6.