Objective:
This systematic review
explores the impact of albuminuria on renal function in patients with type 2
diabetes (T2D), assessing its role in diagnosing diabetic kidney disease (DKD)
and its correlation with reduced glomerular filtration rate (GFR). Materials
and methods: A systematic review was conducted following PRISMA guidelines. Searches in PubMed, Embase, Cochrane Library, and Medline included studies from 2019 to 2023. Inclusion criteria were adults (=18 years) with T2D, studies assessing impact
of albuminuria on kidney function, including randomized controlled trials, observational studies, or meta-analyses. Primary outcomes included albuminuria progression, renal function decline (estimated GFR [eGFR] or creatinine clearance), and DKD progression.
Secondary outcomes evaluated the safety and tolerability of interventions managing albuminuria in T2D patients. Two reviewers independently extracted data and assessed risk of bias. Results: From 1,748 records, nine studies involving 9,91,285
patients were included. Studies consistently showed higher albuminuria levels to be significantly associated with reduced eGFR and increased DKD progression risk. Conclusions:
Our findings underscore albuminuria as a crucial indicator of kidney damage and eGFR as a key marker for DKD severity in T2D patients. This review highlights the need for patient-centered care in managing T2D to reduce renal complications and calls
for further research to comprehensively understand DKD outcomes.
Keywords: Albuminuria, kidney function, glomerular filtration rate, type 2
diabetes, kidney disease, outcomes
Concerns about the possible rise in
demand for health care services, mainly specialized nephrology treatment,
have been expressed due to the greater
frequency of chronic kidney disease (CKD) associated with global population
aging. Declining estimated glomerular filtration rates (eGFR) frequently complicate type 2 diabetes (T2D). About 35% of adult patients who have been diagnosed with T2D have CKD, and they are more vulnerable to end-stage kidney disease (ESKD) owing
to diabetic nephropathy1. Various factors have been considered to be reasons for the declining eGFR among patients who have T2D and the eventual progress of the condition to ESKD. However, the courses of treatment for the conditions have
been heterogeneous and complex due to the diverse characteristics of patients and the specificity of their conditions1.
The severity of CKD is commonly evaluated using
the eGFR, a measure of kidney function, and the albuminuria level, a sign of
kidney damage. To customize CKD care and direct optimal resource allocation,
including faster referral of patients at higher risk of CKD progression, both
eGFR and albuminuria have proved helpful in developing risk-stratification
techniques2. The most common method used to identify albuminuria is
the urine albumin-to-creatinine ratio (UACR). The typical UACR level in spot urine specimens is <30 mg/g3.
The urine total protein-to-creatinine ratio or UPCR (mg/g), is often <0.2 in
adults4. Many situations, such as illness, stress, pregnancy, nutrition, exposure to cold temperatures, and physical activity, can cause a brief increase in urine protein levels. UPCR testing procedure can provide additional information
on kidney function. It is highly accurate and can be used to diagnose kidney illness and monitor diseases that damage the kidneys5,6.
The relationship between albuminuria and
proteinuria is well-documented in CKD.
Albuminuria often accompanies proteinuria, significantly when 24-hour proteinuria surpasses 500 mg2. This relationship is crucial for understanding CKD progression. In cases of glomerular damage, there is an increase in glomerular permeability
to macromolecules, which raises the amount of plasma proteins excreted in the urine. Albumin, with a molecular weight of about 69 kD, is the most common protein expelled in urine under severe glomerular damage conditions. It often makes up over 50%
of the urine proteins. Consequently, albuminuria is the characteristic marker of glomerular proteinuria.
In cases of diabetic glomerulosclerosis,
increases in albuminuria indicate disease progression, even when the
proteinuria rate is within the normal range (e.g., <200 mg/24 h)4. This is a prime example of using
albuminuria to monitor the progression of early glomerular injury. Urine
albumin at concentrations <1 mg/dL can be detected using immunoassays, which help measure low-level changes in albuminuria. These assays show that the standard 24-hour urine albumin excretion is <30 mg albumin/g creatinine4.
Albuminuria rates 30 to 300 mg/g creatinine are termed microalbuminuria. Macroalbuminuria is the term used to describe albuminuria rates above this level. When diabetic
nephropathy reaches the macroalbuminuria level, albumin takes over as the predominant urinary protein, and proteinuria follows albuminuria. The benefit of evaluating albuminuria over proteinuria usually disappears at that time
3.
A slower decline in the eGFR and an improvement
in the renal prognosis are linked to the degree of proteinuria in glomerular
disease, which is intimately connected to CKD progression. Renal function in
eGFR initially declined in response to improvements in albuminuria and
proteinuria6. In addition, rises in the level of urinary proteins,
which are common in cases of albuminuria, have
been related to increased risk of developing coronary heart disease and
creating other health problems in patients with CKD and T2D2. The
link between excessive proteinuria and cardiovascular risks plausibly holds stress on the point of early patient assessment and effective strategy for treating CKD patients7. Therefore, monitoring eGFR and albuminuria is essential for
CKD risk stratification and developing targeted therapeutic strategies. Early intervention and precise monitoring can help manage CKD progression, mitigate associated cardiovascular risks, and improve patient outcomes.
This study aims to
identify the impact of albuminuria on kidney function,
specifically its correlation with eGFR,
among patients with T2D. By examining existing literature, we seek to clarify
the role of albuminuria in predicting DKD progression and highlight the importance
of routine albuminuria assessment in clinical practice.
Subjects
The selection of relevant articles began with
screening based on exclusion and inclusion criteria. Participants eligible for
inclusion were adults aged 18 or older
diagnosed with T2D. The inclusion criteria comprised articles, published in
English, that conducted qualitative and quantitative analyses, articles discussing the impact of albuminuria on kidney function in patients with T2D, and studies published between 2019 and 2023. Included studies assessed interventions targeting
albuminuria and its effect on kidney function. The exclusion criteria encompassed studies falling outside the specified time interval (before 2019 or after 2023) and studies not directly addressing the association between albuminuria and kidney function
in patients with T2D.
Only studies meeting the criteria of
quantitative and qualitative analysis, observational studies, randomized controlled trials, and identification of the
interaction between proteinuria and albuminuria, and its impact on kidney function were included in this research. The selected studies focused on the relationship between abnormal renal function, decreased eGFR, and enhanced UACR. In the
pilot review stage, all retrieved papers were first brought into Endnote 20, and a first de-duplication of the studies was done in it. After retrieving the complete text and any supplementary files, two independent reviewers (THK and XBL) separately
assessed the titles and abstracts, per the mentioned eligibility criteria, using the Rayyan Software. Email correspondence was used to inquire about missing data from the corresponding authors of pertinent articles. For the current review, only publications
that were available in full text were taken into account.
Study Design
The a priori protocol was created and was listed
under PROSPERO CRD42024542353 in the
International Prospective Register of Systematic Reviews. For this review, we followed Preferred Reporting Items for
Systematic Review and Meta-Analysis (PRISMA) reporting criteria to
comprehensively analyze the qualitative and quantitative research examining the
relationship between albuminuria and kidney function in patients with T2D. Figure 1 illustrates the search process flow diagram per the PRISMA guidelines.
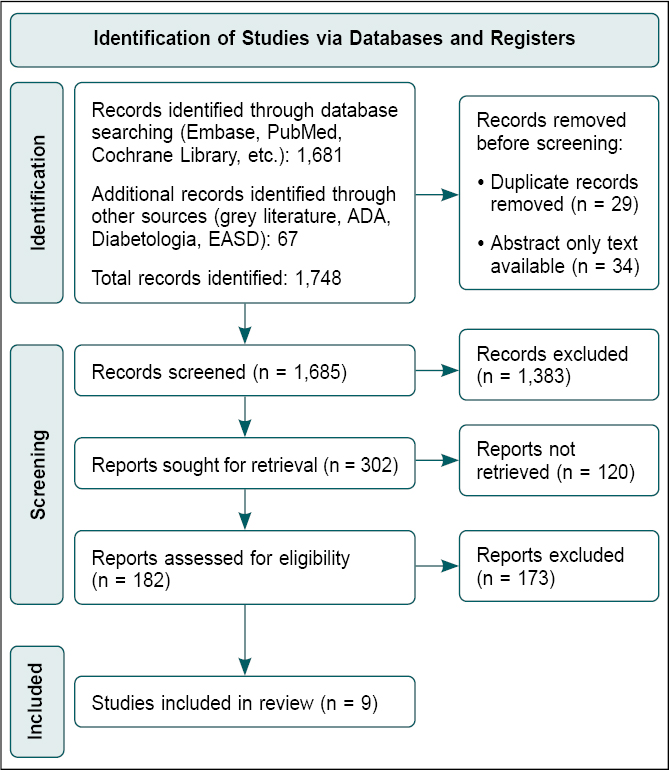
Figure 1. Summary of study search and selection process (PRISMA flow chart).
The search keywords for this research study were
initially selected based on database
exploration. Electronic databases, including Embase, PubMed, global clinical trials, Cochrane Library (incorporating the CENTRAL - Cochrane Central Register of Controlled Trials), and Medline were utilized. CENTRAL and Medline
were targeted explicitly for observational and clinical studies investigating the interaction between albuminuria and kidney function in patients with T2D. We also conducted efforts and attempts to screen the references and citations of published
papers for any possible additional studies. Only studies published in the English language were considered for inclusion.
The search
strategy was optimized and validated in PubMed and then adapted in other databases using keywords, their synonyms, abbreviations, and MeSH terms for “Urine Protein Creatinine Ratio”, “Urine Albumin Creatinine Ratio”, “Proteinuria”, “Albuminuria”, “Glomerular Filtration Rate”, “eGFR”,
“Diabetic Kidney Diseases”, “Chronic Kidney Disease”, “Outcomes”, “Type 2”, “Diabetes Mellitus”, and “T2DM”. Additionally, grey
literature was examined using open grey literature databases, and extra databases were identified for grey literature search, including websites and
records of ADA (American Diabetes Association), Diabetologia, and EASD (European Association for the Study of Diabetes).
Data
Collection
Data extraction and
risk of bias assessment were performed by at least two independent reviewers. Before data extraction, a standardized Excel form was created to capture the following information: study identifier, including author and year of publication, study design, and outcomes.
The risk of bias assessment was evaluated using Cochrane’s Risk of Bias 2 (RoB2) tool and graded as “low-risk”, “some concerns”, or “high-risk” of bias. The RoB2 tool assessed for risk of bias in the following components: (i) randomization process, (ii) any deviation from
intended interventions, (iii) missing outcome data, (iv) measurement of the outcome, (v) selection of the reported result, and (vi) overall RoB. When there were discrepancies between two reviewers, a third reviewer would perform independent data extraction and risk of bias assessment and arbitrate the dispute.
Statistical Analysis
The primary outcomes in this systematic review will focus on the progression of albuminuria, the decline in renal function measured by eGFR or creatinine clearance, and the development or progression of diabetic kidney disease (DKD).
Secondary outcomes involve evaluating the safety and tolerability of these interventions in managing albuminuria and preserving kidney function in patients with T2D. Only data presented using the intention-to-treat (ITT) principle were extracted
for the efficacy outcomes. Meanwhile, only data presented using each study’s safety analysis set (SAS) were extracted for the safety outcomes.
The initial search (Fig. 1) yielded 1,748 articles. Duplicates (n = 29) and articles that did not have full texts
available (n = 34) were removed, leaving 1,685 articles. This was then screened using the study objective and design to remove 1,503 articles further, leaving 182 articles. Eligibility criteria were then applied to remove 174 articles further. This study included nine articles involving 9,91,285 patients with T2D, identifying albuminuria and kidney function as essential outcomes.
Table 1 provides a summary of these studies, highlighting their key findings regarding the
association between albuminuria and kidney function outcomes such as eGFR and progression to DKD1-3,5-10. The studies consistently demonstrate that higher levels of albuminuria are significantly associated with reduced eGFR and an increased
risk of DKD progression.
|
Table 1. Summary of Studies and their Kidney Function
Outcomes1-3,5-10
|
|
Study Title
|
Authors
|
Year
|
Study Design
|
Location
|
Sample Size
|
Purpose
|
Outcomes
|
|
Liver Stiffness, Albuminuria, and Chronic Kidney Disease in Patients with NAFLD: A Systematic Review and Meta-Analysis
|
Ciardullo et al2
|
2022
|
Systematic review and meta-analysis
|
Italy
|
7,736 participants from 7 studies
|
To assess the association between liver stiffness, albuminuria, and CKD
in patients with NAFLD.
|
Elevated UACR (=30 mg/g) in NAFLD patients is associated with higher
CKD prevalence and reduced eGFR.
|
|
Diabetic Kidney Disease Benefits from Intensive Low-Protein Diet: Updated
Systematic Review and Meta-Analysis
|
Li et al6
|
2021
|
Systematic review and meta-analysis
|
China
|
506 participants from 9 studies
|
To assess the evidence-based efficacy of a low-protein diet in the
management of DKD.
|
Proper DPI is suggested for adults, but in low amounts, to reduce renal
function complications. A DPI =0.8 g/kg/day can positively impact renal
function, reducing the risk of kidney failure by controlling proteinuria.
|
|
Diagnostic Accuracy of Urine Dipstick Testing for Albumin-to-Creatinine
Ratio and Albuminuria: A Systematic Review and Meta-Analysis
|
Mejia et al3
|
2021
|
Systematic review and meta-analysis
|
Peru
|
37,435 patients from 14 studies
|
To evaluate the diagnostic accuracy of urine dipstick tests for
albuminuria.
|
Urine dipstick tests are helpful for initial screening but have
limitations in sensitivity and specificity for detecting elevated
albuminuria.
|
|
The Level of Serum Albumin is Associated with Renal Prognosis and Renal
Function Decline in Patients with Chronic Kidney Disease
|
Cheng et al8
|
2023
|
Prospective Cohort
|
China
|
754 patients
|
To investigate the relationship between serum
albumin levels and
renal prognosis in CKD patients.
|
Lower serum albumin levels (<3.5 g/dL) are associated with faster
renal function decline and poorer renal prognosis.
|
|
Lifestyle Interventions, Kidney Disease Progression, and Quality of Life:
A Systematic Review and Meta-Analysis
|
Neale et al9
|
2023
|
Systematic review and meta-analysis
|
Australia
|
15,288 participants from 68 studies
|
To determine the impact of lifestyle interventions on CKD progression and
quality of life.
|
Lifestyle interventions, including exercise and diet, improved eGFR and
reduced albuminuria, slowing CKD progression.
|
|
Conversion of Urine Protein-Creatinine Ratio or Urine Dipstick Protein
to Urine Albumin-Creatinine
Ratio for Use in Chronic Kidney Disease Screening and Prognosis: An Individual
Participant-based Meta-Analysis
|
Sumida et al10
|
2020
|
Meta-analysis
|
United States
|
9,19,383 patients across 33 studies
|
To evaluate the effectiveness of converting UPCR or urine dipstick
protein to UACR for CKD screening and prognosis.
|
Albumin levels can indicate the status of patients with CKD. Converting
UPCR or urine dipstick protein to UACR is effective for CKD screening and
prognosis.
|
|
Effects of Exercise Training on Proteinuria in Adult Patients with
Chronic Kidney Disease:
A Systematic Review and Meta-Analysis
|
Yang et al5
|
2020
|
Systematic review and meta-analysis
|
China
|
623 CKD patients from 11 studies
|
To assess the effects of exercise training on proteinuria in CKD
patients.
|
Regular exercise training
does not aggravate proteinuria in adult CKD patients and also
significantly reduces proteinuria levels.
|
|
Rate of Kidney Function Decline and Factors Predicting Progression of
Kidney Disease in Type 2 Diabetes Mellitus Patients with Reduced Kidney
Function: A Nationwide Retrospective Cohort Study
|
Kaewput et al1
|
2020
|
Retrospective cohort
|
Thailand
|
8,464 T2D patients
|
To determine the relationship between albuminuria levels and CKD
progression in T2D patients.
|
Higher albuminuria levels (>300 mg/day)
significantly correlated with rapid eGFR decline, predicting faster CKD
progression.
|
|
Prevalence and Risk Factors of Chronic Kidney Disease among Type 2
Diabetes Patients: A Cross-Sectional Study in Primary Care Practice
|
Jitraknatee et al7
|
2020
|
Cross-sectional
|
Thailand
|
1,096 T2D patients
|
To identify the prevalence and risk factors of CKD in T2D patients in
primary care.
|
Risk factors for CKD include retinopathy, HbA1c =7%, anemia, and
albuminuria significantly associated with decreased eGFR.
|
NAFLD = Nonalcoholic fatty liver disease; CKD = Chronic kidney disease; UACR = Urine albumin-to-creatinine ratio; eGFR = Estimated glomerular filtration rate; DKD = Diabetic kidney disease; DPI = Dietary protein intake; UPCR = Urine protein-to-creatinine
ratio; T2D = Type 2 diabetes; HbA1c = Glycated hemoglobin.
Kaewput et al1 conducted a nationwide
retrospective cohort study and found a
significant correlation between high levels of albuminuria and rapid eGFR decline, indicating that higher albuminuria predicts faster CKD progression. Li et al6 discovered that a proper dietary protein intake (DPI) of =0.8 g/kg/day is
suggested for adults to reduce renal function complications, including the risk of kidney failure, by controlling proteinuria. Similarly, Ciardullo et al2 identified elevated albuminuria levels in patients with CKD characterized by UACR
=30 mg/g and eGFR <60 mL/min, signifying an increased risk of kidney function deterioration.
Jitraknatee et al7 conducted a
cross-sectional study in primary care practice and identified several predictors of eGFR decrease, including retinopathy, glycated hemoglobin (HbA1c)
=7%, and anemia, emphasizing the complex risk profile of T2D patients. Mejia et al3 evaluated the diagnostic accuracy of urine dipstick testing for albumin-to-creatinine ratio and albuminuria, highlighting its limitations in reliably identifying elevated albuminuria.
Cheng et al8 explored the association between serum albumin levels and renal progression in CKD, demonstrating
that lower serum albumin is linked with faster renal function decline. Neale et al9 investigated lifestyle interventions and found that exercise practices improve creatinine and eGFR, while dietary interventions contribute to improvements in albuminuria.
Sumida et al10 conducted a meta-analysis on converting UPCR or urine dipstick protein to UACR, showing that albumin levels can effectively indicate the status of patients with CKD. Lastly, Yang et al5 reviewed the effects of exercise training on
proteinuria in CKD patients, confirming that regular exercise has positive effects on reducing proteinuria.
Proteinuria predicts future GFR reduction and ESKD onset in population-based studies and controlled trials. When there is overt proteinuria in both diabetic and nondiabetic renal disease, a reduction in proteinuria inevitably results in protection against decreased renal function. A person may have renal disease even if their eGFR is 60 or above if they have albumin in their urine11. Various research studies have
investigated how dietary interventions help improve the condition of albuminuria9. In another study, even when traditional cardiovascular risk factors were considered, there was a nearly 2.6-fold increase in the risk of death for those with a significant decline in eGFR (<45 mL/min/1.73 m2) in addition to proteinuria12.
The study by
Kaewput et al1 showed essential data on the severity of CKD in T2D patients and the crucial role of albuminuria in predicting kidney function. The research contained patients with deteriorated kidney function (baseline eGFR between 15 to 59 mL/min/1.73 m²). These results demonstrate an association between albuminuria and a higher chance of eGFR
decline. This indicated that the more albuminuria, the faster CKD will progress to the later stages, such as CKD stage 5 or dialysis.
According to Jitraknatee et al7, even in primary care, the failure rate of kidneys is relatively standard among T2D patients, and the severity levels may vary from different stages. Regarding risk factors, the study’s multivariable logistic regression analysis found several predictors significantly correlated with eGFR decrease, such as
retinopathy, HbA1c =7%, and anemia. These aspects, inclusive of albuminuria, indicate that patients with T2D tend to have a complex risk profile7.
It is essential to mention these risk factors because the integrated approach to managing the decline of eGFR in patients with diabetes is not limited to kidney function. It is also taking into account different diabetes-related complications. This comprehensive awareness sets the stage for developing target-oriented therapies and monitoring protocols to prevent higher levels of eGFR reduction. Another study also showed that various risk factors may be related to an ongoing decline in eGFR. Besides albuminuria, other factors such as duration of diabetes, systolic blood pressure, and serum uric acid are associated with an increasing risk of eGFR worsening13.
This manuscript’s qualitative and quantitative studies shed light on the intricate relationship between albuminuria, renal function, and cardiovascular outcomes in T2D patients. The UACR emerges as a critical diagnostic tool, aiding
in identifying renal impairment and disease progression. Despite its significance, further research is warranted to enhance the reliability and accuracy of UACR testing in clinical practice.
Additionally, the correlation between albuminuria and rapid eGFR decline underscores the importance of routine check-ups and early diagnosis in postponing CKD progression in T2D patients. Identifying risk factors for eGFR decline, including retinopathy, HbA1c levels, and anemia, enables the formulation of personalized treatment strategies to
mitigate CKD progression and improve overall health outcomes.
Moreover, interventions targeting factors associated with slower CKD progression, such as aging and renin-angiotensin-aldosterone system (RAAS) inhibitors, offer promising avenues for disease management. Integrating preventive measures into clinical care, including early diagnosis of albuminuria and awareness of risk factors, can significantly impact long-term outcomes for T2D patients by minimizing CKD progression and improving overall quality of life.
Heterogeneity among the included studies may be considered a severe limitation of the present systematic review on albuminuria and kidney function in T2D patients. Differences in study design, patient populations, and targeted interventions on albuminuria undoubtedly jeopardize generalization. Furthermore, reliance on electronic databases for the search and the restriction of the review to English-language studies probably predispose the selection and may reduce the scope of the review. Another source of variance
among the results reported in studies could be the variation in the definition and methods of measurement chosen by the different studies for albuminuria and
kidney function. Moreover, publication bias cannot be excluded, as studies with negative or inconclusive results are less likely to be published. Future
research is, therefore, needed to overcome these limitations by defining the standard definition, broadening the inclusion criteria, and incorporating the broadest possible range of studies.
A comprehensive approach to managing declining eGFR in T2D patients therefore involves early diagnosis of albuminuria, awareness of risk factors, personalized treatment strategies, and integration of preventive measures into clinical care. Further research is warranted to enhance diagnostic tests’ reliability and accuracy and explore
additional interventions for mitigating CKD progression and improving long-term outcomes in T2D patients.
Our findings highlight the importance of investigating albuminuria’s impact on eGFR among individuals with T2D. The studies reviewed indicated a strong association between higher albuminuria levels and reduced eGFR, underscoring albuminuria’s role as a crucial marker in assessing DKD severity. This review emphasizes the necessity for tailored,
patient-centered care in managing T2D to reduce renal complications. Further studies are needed to evaluate DKD outcomes in this context comprehensively, and health care providers should consider albuminuria levels when developing treatment strategies for T2D patients to mitigate the progression of renal disease.
Funding: This publication was prepared without any external source of funding.
Author Contribution: MM contributed to ideas, concepts, supervision, and validation. THK contributed to the analysis and wrote the first draft of the study. XBL contributed to writing part of the contents and table. All authors reviewed and edited the manuscript and approved it for submission.
Acknowledgments: Not applicable.
Conflicts of Interests: Not applicable.
Ethical Approval: Ethical approval was not necessary for the preparation of this article.
1.
Kaewput W, Thongprayoon C, Chewcharat A, Rangsin R, Satirapoj B, Kaewput C, et al. Rate of kidney function decline and factors predicting progression of kidney disease in type 2 diabetes mellitus patients with reduced kidney function:
a nationwide retrospective cohort study. Ther Apher Dial. 2020;24(6):677-87.
2.
Ciardullo S, Ballabeni C, Trevisan R, Perseghin G. Liver stiffness, albuminuria and chronic kidney disease in patients with NAFLD: a systematic review and meta-analysis. Biomolecules. 2022;12(1):105.
3.
Mejia JR, Fernandez-Chinguel JE, Dolores-Maldonado G, Becerra-Chauca N, Goicochea-Lugo S, Herrera-Añazco P, et al. Diagnostic accuracy of urine dipstick testing for albumin-to-creatinine ratio and albuminuria: a systematic review
and meta-analysis. Heliyon. 2021;7(11):e08253.
4.
Yue H, Zhou P, Xu Z, Liu L, Zong A, Qiu B, et al. Effect of low-protein diet on kidney function and nutrition in nephropathy: a systematic review and meta-analysis of randomized controlled trials. Clin Nutr. 2020;39(9):2675-85.
5.
Yang L, Wu X, Wang Y, Wang C, Hu R, Wu Y. Effects of exercise training on proteinuria in adult patients with chronic kidney disease: a systematic review and meta-analysis. BMC Nephrol. 2020;21(1):172.
6.
Li Q, Wen F, Wang Y, Li S, Lin S, Qi C, et al. Diabetic kidney disease benefits from intensive low-protein diet: updated systematic review and meta-analysis. Diabetes Ther. 2021;12(1):21-36.
7.
Jitraknatee J, Ruengorn C, Nochaiwong S. Prevalence and risk factors of chronic kidney disease among type 2 diabetes patients: a cross-sectional study in primary care practice. Sci Rep. 2020;10(1):6205.
8.
Cheng T, Wang X, Han Y, Hao J, Hu H, Hao L. The level of serum albumin is associated with renal prognosis and renal function decline in patients with chronic kidney disease. BMC Nephrol. 2023;24(1):57.
9.
Neale EP, Rosario VD, Probst Y, Beck E, Tran TB, Lambert K. Lifestyle interventions, kidney disease progression, and quality of life: a systematic review and meta-analysis. Kidney Med. 2023;5(6):100643.
10.
Sumida K, Nadkarni GN, Grams ME, Sang Y, Ballew SH, Coresh J, et al; Chronic Kidney Disease Prognosis Consortium. Conversion of urine protein-creatinine ratio or urine dipstick protein to urine albumin-creatinine ratio for use in chronic
kidney disease screening and prognosis: an individual participant-based meta-analysis. Ann Intern Med. 2020;173(6):426-35.
11.
Chun KJ, Jung HH. SGLT2 inhibitors and kidney and cardiac outcomes according to estimated GFR and albuminuria levels: a meta-analysis of randomized controlled trials. Kidney Med. 2021;3(5):732-44.
12.
Nakamura K, Sasaki T, Yamamoto S, Hayashi H, Ako S, Tanaka Y. Effects of exercise on kidney and physical function in patients with non-dialysis chronic kidney disease: a systematic review and meta-analysis. Sci Rep. 2020;10(1):18195.
13.
Zhang X, Fang Y, Zou Z, Hong P, Zhuo Y, Xu Y, et al. Risk factors for progression of CKD with and without diabetes. J Diabetes Res. 2022;2022:9613062.