Background:
The International
Classification of Diseases (ICD) has described constipation as decrease in
normal frequency of defecation accompanied by difficult or incomplete passage
of stool and/or passage of excessively hard, dry stool (ICD10-CM-K59). Overall,
the average prevalence of constipation in adults has been estimated as 16%
worldwide (varies between 0.7% and 79%); in adults aged 60 to 110 years, the
prevalence has been estimated to be 33.5%. Objective: To evaluate and
compare the efficacy of tablet Anuloma DS and lactitol + ispaghula powder in
constipation. Materials and methods: Sixty-two subjects with
constipation were divided into two groups: Group A with 32 subjects and Group B
with 30 subjects. Group A received 1 Anuloma DS tablet at bedtime and
Group B received lactitol + ispaghula powder 5 g at bedtime for 15 days. Results:
Twenty-eight patients in Group A showed significant improvement in stool
consistency, whereas just 8 patients showed improvement in consistency of
stool in Group B. Twenty patients showed improvement in frequency of stool in
Group A, whereas only 3 patients showed this improvement in Group B.
Twenty-nine patients in Group A reported good improvement in feeling after
defecation compared to 9 patients in Group B. Pain in abdomen improved in 21
patients in Group A versus 9 patients in Group B. Improvements were also seen
in scores on the Constipation Assessment Scale, Patient Assessment Scale, and
Quality of Life Questionnaire. Conclusion: Anuloma DS showed significant
clinical benefits in the treatment of constipation compared to lactitol +
ispaghula powder.
Keywords: Anuloma DS, constipation, Constipation Assessment Scale, ispaghula,
lactitol
The fast-paced, lifestyle adopted by many
individuals in today’s competitive society has had a significant impact on the health of the gastrointestinal tract resulting in a rising prevalence of gastrointestinal disorders.
Constipation, or Vibandha, is one such
outcome. Vibandha is not mentioned in Ayurvedic texts as a specific
disease but has been mentioned as a Nidana (causative factor), Lakshana
(symptoms), and Upadrava (complications) of several diseases. It can be
considered as a Lakshana in Udavarta (retention of feces, flatus,
and urine) like Anaha (obstruction), Adhmana
(distension), Malaavastamba (hardness of feces) due to the Pratiloma
Gati (reverse flow) of Apana Vayu1.
Vibandha (constipation)
is the obstruction of the Purisha (feces)
in the Purishavaha Srotas (excretory system). Constipation is a warning sign for many current or imminent disorders.
The International
Classification of Diseases, (ICD10-CM-K59), defines constipation as the
decrease in normal frequency of defecation accompanied by difficult or incomplete passage of stool and or passage of
excessively hard and dry stool. The prevalence of constipation in India is
estimated to be 16.8% and that of self-reported constipation is 24.8%2.Overall, the average prevalence of constipation in adults has been
estimated to be 16% worldwide (varies between 0.7% and 79%), whereas the
prevalence in adults aged 60 to 110 years was 33.5%3.
Epidemiological studies show that the prevalence of constipation increases with
the age and is more common in women than in men4.
Various pharmacological agents such as bulk
laxatives, stimulant laxatives, stool softeners, osmotic agents, lubricant
laxatives, suppositories, and enema are used in clinical practice to treat
constipation. However, their long-term use may cause electrolyte disturbance,
dehydration and mineral deficiencies, and may even produce drug dependency.
Hence, there is a need for an alternative
therapeutic approach, which not only manages the condition, but also minimizes
the recurrence of symptoms.
Anuloma DS is an Ayurvedic proprietary medicine
that contains different medicinal plants such as Cassia lanceolata (Senna), Apium leptophyllum (Ajamoda), Cuminum cyminum (Cumin or Jeeraka), Terminalia chebula (Haritaki), Glycyrrhiza glabra (Liquorice), Zingiber officinale (Ginger or Shunti), and Halite (Rock salt). These drugs are Agnideepaka (increase the digestive fire), Katu
Rasa (pungent taste), Ushna Veerya (hot potency), and Katu Vipaka5.
The primary objective of this comparative study
was to evaluate the efficacy of Anuloma DS tablet and lactitol + ispaghula
powder in relieving constipation. Improvements in the Quality of Life
Questionnaire, Constipation Assessment Scale, and Patient Assessment Scale were
the secondary objectives of the study.
The study designed as an open-label comparative
double arm clinical study enrolled 62 subjects visiting medicine OPDs of our
hospital for the treatment of constipation. After screening, eligible subjects
were instructed to take either Anuloma DS 1 tablet at bedtime with warm water
or lactitol + ispaghula powder 5 g at bedtime with warm milk for a period of 15
days.
The inclusion criteria were male and female
adults aged 18 to 70 years, who were suffering from functional constipation,
were willing to sign consent form and were able to present for follow-ups.
The primary study
objective assessed changes in symptoms of constipation such as consistency of stool,
frequency of stool, nature of evacuation, pain in abdomen, generalized
weakness, headache, body ache, and muscle cramps. Secondary end points were
changes in the Constipation Assessment Scale, which evaluates 8 domains such as
abdominal distension, change in amount of gas pass rectally, less frequent
bowel movement, oozing of liquid stool, rectal fullness, rectal pain, small
stool size, and urge but inability to pass stool. Patient assessment of
constipation contain 12 domains such as discomfort- pain-bloating in abdomen,
stomach cramp, painful bowel movement, rectal burning, rectal bleeding,
incomplete bowel movement, hard bowel movement, small bowel movement, straining
to pass bowel movement, and false alarm. And the Patient Assessment of
Constipation Quality of Life (PAC-QOL) questionnaire is a brief but
comprehensive tool, which evaluates constipation through daily individual
health assessment and functioning.
Constipation was diagnosed based on the Rome IV
criteria6 as follows:
·
Fewer than 3 spontaneous bowel movements per week.
·
Straining for more than 25% of defecation attempts.
·
Lumpy or hard stools for more than 25% defecation attempts.
·
Sensation of anorectal obstruction or blockage for more than 25% of defecation attempts.
·
Sensation of incomplete defecation for more than 25% of defecation attempts.
·
Manual maneuvering required to defecate for more than 25% of defection attempts.
Exclusion criteria
were the presence of irritable bowel syndrome,
inflammatory bowel disorder, colon carcinoma,
medication known to cause
constipation (opioid analgesics, antidepressants, anticonvulsants, amitriptyline), uncontrolled systemic ailments or neurological
illness, pregnancy and lactation.
The study
participants were evaluated at baseline and two assessment points (Visit 1- Day
1 and Visit 2- Day 15). Patients underwent history and physical
examination at all assessments points. They were also enquired about
constipation signs and symptoms and evaluated with the Constipation Assessment
Scale, Patient Assessment Scale, and Quality of Life Questionnaire. Concomitant
medication and adverse events were also assessed.
Data comparison between baseline and follow-up
visit was performed using a Friedman test, Wilcoxon signed rank test,
Mann-Whitney test, unpaired and paired t-tests. A p value of 0.05 was
considered statistically significant. Statistical analysis was done using
statistical software SPSS 21.0.
A total of 62 subjects were enrolled in the
study. Two subjects were dropped as they did not come for follow-up. Hence, 60
subjects were included in the final analysis. Age-wise distribution of subject
shows that 28 subjects belong to the age group 18 to 27 years, while 10
subjects belonged to 48 to 57 years. Out of 60 subjects, 34 were females and 26
were males. Thirty-eight subjects belonged to middle class and the diet-wise
distribution showed equal number in both vegetarian and mixed diet. Table 1
describes the demographic characteristics of the participants.
|
Table 1. Demographic Data of the Enrolled Subjects (n =
60)
|
|
Age (years)
|
Group A (Anuloma DS)
|
Group B (Lactitol + Ispaghula)
|
|
18-27
28-37
38-47
48-57
58-67
|
15
2
3
3
7
|
13
4
4
7
2
|
|
Gender
Male
Female
|
Group A
13
17
|
Group B
13
17
|
|
Diet
Mixed
Vegetarian
|
Group A
15
15
|
Group B
18
12
|
Assessment of Signs and Symptoms of Constipation
Constipation symptoms such as reduced appetite,
distension of abdomen, pain in abdomen, general weakness, headache, body ache,
muscle cramps, consistency of stool, frequency of stool, nature of evacuation,
feeling after defecation were assessed on a 4-point scale. The mean symptom
scores were significantly improved in Group A compared to Group B as shown
in Tables 2 & 3 and Figure 1.
|
Table 2. Comparison of Mean Changes in Symptom Score from
V1 and V2 (n = 60)
|
|
Parameters
|
Group A (Study Group)
|
|
Group B (Control Group)
|
|
Visit
|
Mean score (Mean ± SD)
|
P value
|
Visit
|
Mean score (Mean ± SD)
|
P value
|
|
Reduced appetite
|
V1
V2
|
1.40 ± 0.724
0.47 ± 0.507
|
0.00
|
V1
V2
|
1.17 ± 0.747
1.13 ± 0.730
|
0.317
|
|
Distension of abdomen
|
V1
V2
|
1.43 ± 0.626
0.40 ± 0.498
|
0.00
|
V1
V2
|
1.33 ± 0.711
1.10 ± 0.712
|
0.01
|
|
Pain in abdomen
|
V1
V2
|
0.93 ± 0.785
0.20 ± 0.484
|
0.00
|
V1
V2
|
0.70 ± 0.750
0.40 ± 0.498
|
0.003
|
|
Generalized weakness
|
V1
V2
|
1.03 ± 0.850
0.23 ± 0.430
|
0.00
|
V1
V2
|
0.90 ± 0.885
0.57 ± 0.679
|
0.002
|
|
Headache
|
V1
V2
|
0.57 ± 0.858
0.10 ± 0.403
|
0.00
|
V1
V2
|
0.50 ± 0.777
0.33 ± 0.606
|
0.03
|
|
Body ache
|
V1
V2
|
0.60 ± 0.770
0.10 ± 0.305
|
0.00
|
V1
V2
|
0.53 ± 0.937
0.37 ± 0.669
|
0.03
|
|
Muscle cramps
|
V1
V2
|
0.57 ± 0.898
0.17 ± 0.461
|
0.00
|
V1
V2
|
0.80 ± 1.031
0.60 ± 0.814
|
0.01
|
|
Stool consistency
|
V1
V2
|
2.27 ± 0.583
1.10 ± 0.305
|
0.00
|
V1
V2
|
2.17 ± 0.531
1.90 ± 0.607
|
0.01
|
|
Stool frequency
|
V1
V2
|
1.37 ± 0.556
1.00 ± 0.00
|
0.00
|
V1
V2
|
1.20 ± 0.407
1.10 ± 0.305
|
0.08
|
|
Nature of evacuation
|
V1
V2
|
2.33 ± 0.479
1.27 ± 0.450
|
0.00
|
V1
V2
|
2.30 ± 0.535
2.07 ± 0.640
|
0.01
|
|
Feeling after defecation
|
V1
V2
|
2.30 ± 0.466
1.20 ± 0.407
|
0.00
|
V1
V2
|
2.30 ± 0.596
2.00 ± 0.695
|
0.01
|
|
|
|
|
|
|
|
|
|
Table 3. Comparison of Mean Changes in Symptom Score (n =
60)
|
| |
Reduced appetite
|
Distension of abdomen
|
Pain in abdomen
|
Generalized weakness
|
Headache
|
| |
Group A
|
Group B
|
Group A
|
Group B
|
Group A
|
Group B
|
Group A
|
Group B
|
Group A
|
Group B
|
|
MR
|
23.2
|
37.8
|
22.7
|
38.3
|
27.2
|
33.8
|
26.65
|
34.35
|
27.5
|
33.4
|
|
SR
|
695.0
|
1135.0
|
681.0
|
1149.0
|
816.0
|
1014.0
|
799.5
|
1030.0
|
827.0
|
1003.0
|
|
P
|
0.0
|
0.00
|
0.06
|
0.04
|
0.05
|
| |
Body ache
|
Muscle cramps
|
Stool consistency
|
Stool frequency
|
Nature of evacuation
|
Feeling of defecation
|
|
| |
Group A
|
Group B
|
Group A
|
Group B
|
Group A
|
Group B
|
Group A
|
Group B
|
Group A
|
Group B
|
Group A
|
Group B
|
|
|
MR
|
27.8
|
33.1
|
26.3
|
34.7
|
20.3
|
40.7
|
29.0
|
32.0
|
21.1
|
39.9
|
21.3
|
39.3
|
|
|
SR
|
835.5
|
994.5
|
789.0
|
1041.0
|
609.0
|
1221.0
|
870.0
|
960.0
|
632.0
|
1198.0
|
639.0
|
1191.0
|
|
|
P
|
0.08
|
0.02
|
0.00
|
0.08
|
0.00
|
0.00
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
MR = Mean Rank; SR
= Sum Rank; P = P value.
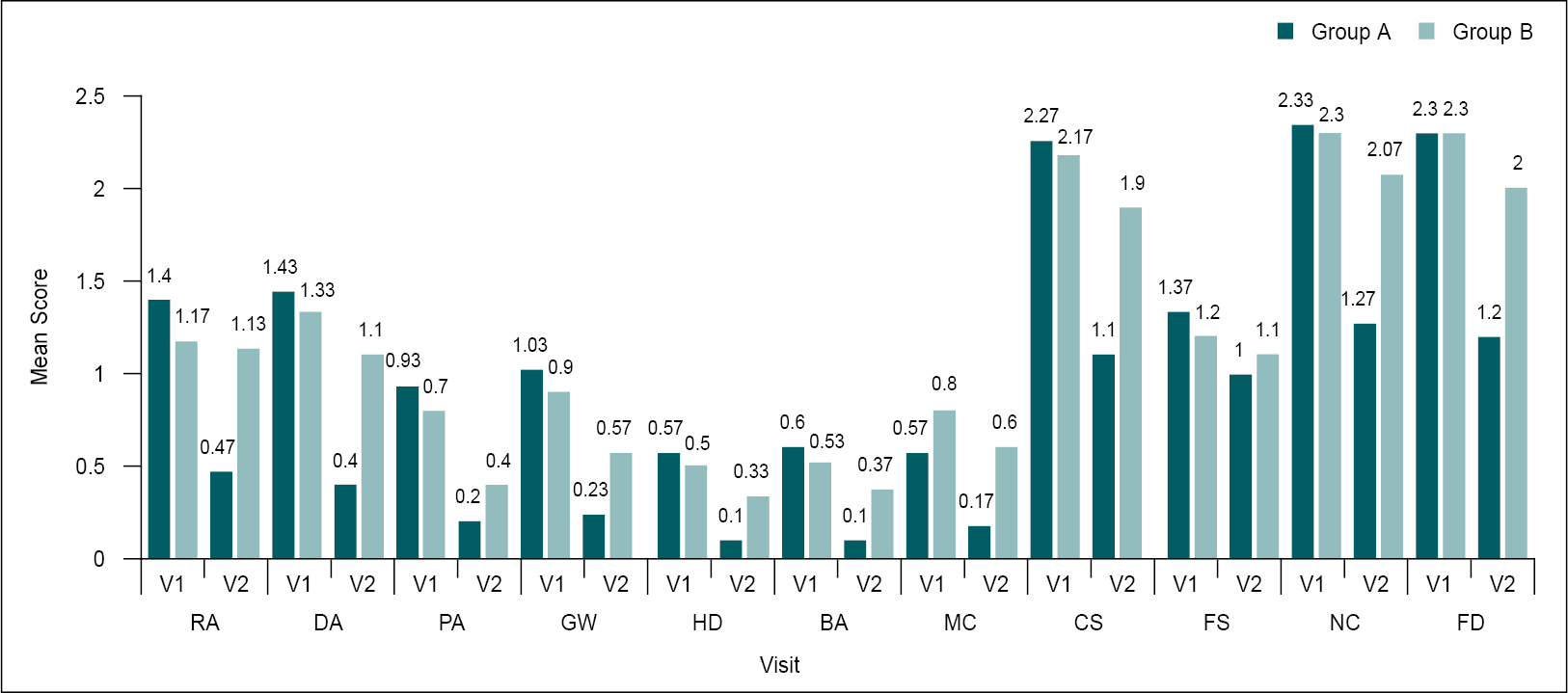
Figure 1. Comparison of mean changes in symptom score from V1 to V2 (n = 60).
RA = Reduced appetite; DA = Distension of abdomen; PA = Pain in
abdomen; GW = Generalized weakness; HD = Headache; BA = Body ache; MC: Muscle
cramps; CS = Stool consistency; FS = Stool frequency; NC = Nature of
evacuation; FD = Feeling after defecation.
Constipation
Assessment Scale and Patient Assessment Scale
Significant improvements were observed in the
Constipation Assessment Scale and Patient Assessment Scale in Group A (Anuloma
DS) (p < 0.00) (Table 4 and Fig. 2).
|
Table 4. Comparison of Mean Changes in Constipation
Assessment Scale and Patient Assessment Scale from V1 to V2 (n = 60)
|
|
Parameters
|
Group A
|
|
Group B
|
|
Visit
|
Mean ± SD
|
SE
|
P value
|
|
Visit
|
Mean ± SD
|
SE
|
P value
|
|
Constipation Assessment Scale
|
V1
V2
|
5.03 ± 2.13
1.73 ± 1.20
|
0.388
0.225
|
<0.00
|
V1
V2
|
5.77 ± 2.72
5.60 ± 2.64
|
0.498
0.483
|
0.02
|
|
Patient Assessment Scale
|
V1
V2
|
11.8 ± 6.08
6.0 ± 3.37
|
1.110
0.061
|
<0.00
|
V1
V2
|
12.3 ± 5.37
11.9 ± 5.10
|
0.981
0.931
|
0.002
|
|
|
|
|
|
|
|
|
|
|
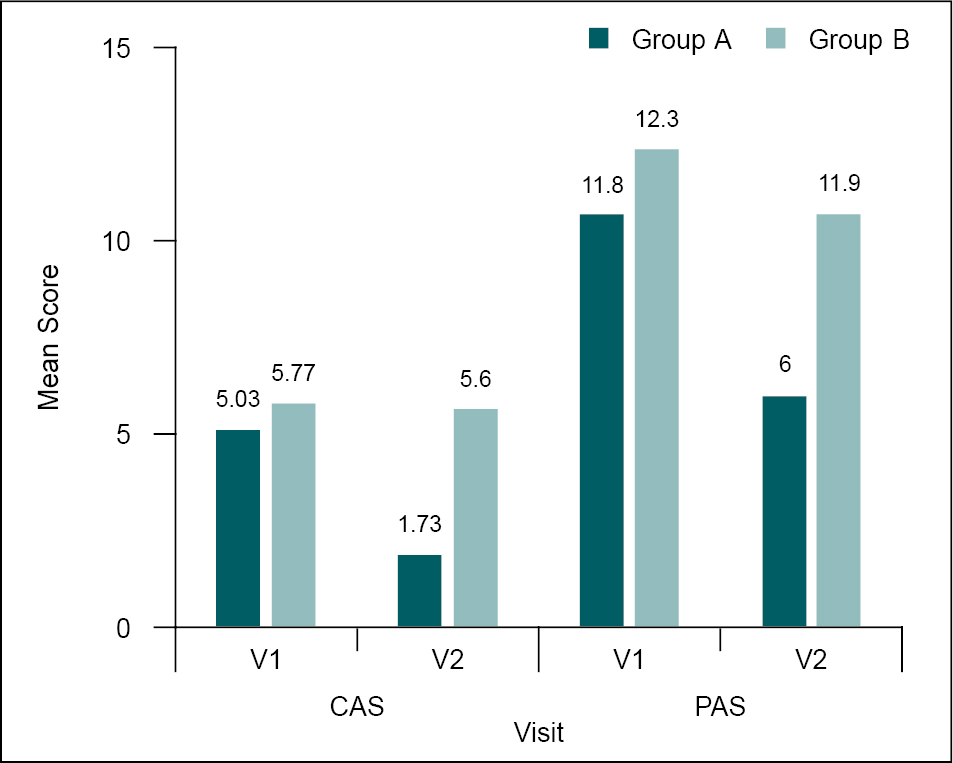
Figure 2. Comparison
of mean changes in Constipation Assessment Scale and Patient Assessment Scale
from V1 to V2 (n = 60).
CAS = Constipation
Assessment Scale; PAS = Patient Assessment Scale.
Assessment of
Quality of Life
Group A had significantly greater improvement in
quality of life than Group B as assessed via the Quality of Life Questionnaire
(Table 5).
|
Table 5. Comparison of Mean Changes in Quality of Life
(PAC-QOL) from V1 to V2 (n = 60)
|
|
Parameters
|
Group A
|
|
Group B
|
|
Visit
|
Mean ± SD
|
SE
|
P value
|
|
Visit
|
Mean ± SD
|
SE
|
P value
|
|
Quality of life
|
V1
V2
|
50.6 ± 13.2
29.9 ± 10.3
|
2.404
1.886
|
<0.00
|
V1
V2
|
49.5 ± 12.4
33.8 ± 11.4
|
2.235
2.083
|
0.001
|
|
|
|
|
|
|
|
|
|
|
SD = Standard
deviation; SE = Standard error.
Constipation is a common condition that affects
people of all ages. It is often erroneously attributed to the natural aging
process. Although aging is associated with changes in the gastrointestinal
tract and may predispose one to develop constipation, the disorder usually has
a multifactorial etiology.
Etiologically, constipation can be broadly
divided into two main groups: primary and secondary7. Primary
or functional constipation is defined as constipation for more than 6
months8, which is not due to any underlying cause such as
medication side effect or an underlying medical condition. It can be
distinguished from irritable bowel syndrome based on the absence of abdominal
pain. It is the most prevalent type of constipation
and frequently has multiple causes. Diets, such as consuming too little fiber or water, or behaviors such as engaging in less physical activity are the main culprits9.
The incidence of gastrointestinal diseases had
an unprecedented hike in recent years. This is mainly due to changes in lifestyle, food habits, behavioral changes, etc. Annavaha
Sroto dushti Vikaras (disease of gastrointestinal system) explained in
Ayurveda classics share similarity with gastrointestinal disorders in terms of
etiopathogenesis and symptomatology. Vibandha (constipation) is a
disease of Annavaha Srotas (gastrointestinal system) caused by
disturbances of Agni (digestive fire). Irregular dietary habits, behavioral changes, stress, etc. lead to Agnimandya (weakened digestive fire), which causes Ajeerna (indigestion) and then constipation.
Abnormalities of Samana (kindling vata)
– Apana Vayu (descending vata), Pachaka Pitta (digesting pitta),
and Kledaka Kapha (moistening kapha) also play significant roles
in causing constipation. Along with the difficulty in passing stools, other
symptoms like pain in abdomen, flatulence, rectal pain, hemorrhoids, headache
can also be associated with constipation. Chronic uncontrolled cases of
constipation can lead to complications like Udavarta, Vataja gulma,
Vatodara.
Management of constipation includes correction
of Agni, movement of Apana Vata and normalizing the vitiated Pachaka
Pitta and Kledaka Kapha. Different formulations like Churna, Kashaya,
Arishta, Ghrita are indicated in the management of Vibandha.
Management of constipation in contemporary
medicine includes lifestyle modifications such as introduction of high-fiber
diet, plenty of water intake, physical exercise, and good bowel habits. Various
classes of laxative medications include fiber supplements, osmotic laxatives,
stimulant laxatives, lubricants, stool softeners, etc. Enemas and suppositories
are used when the above treatments yield no result10.
Various studies report that women are more than
twice as likely to develop constipation as men. This is attributed to the
slower gut transit in women due to the changing levels of progesterone and
estrogen or damage to the pelvic floor in a women’s obstetric history.
Considering the socioeconomical background and
dietary habits of the locality, it is not possible to draw any conclusions. Out
of 60 subjects, 22 were of Vata-Kapha Prakriti and 16 were of Vata-Pitta
Prakriti. Vibandha (constipation) is a Vata-Dosha Pradhana Vyadhi
(main disease), which may be common among people with Vata-predominant
Prakriti.
In this study,
patients in Group A (Anuloma DS tablet) showed significant improvement in primary and
secondary outcome measures compared to Group B (lactitol + ispaghula powder) after 15 days of
intervention.
Appetite was improved in 26 subjects of the
study group and remained same in 4 subjects. In the control group, appetite
improved in 1 subject, but remained same in 29 subjects of the control group.
Anuloma DS contains Agnideepaka herbs like Ajamoda, Shunti and
Jeeraka, Katu Rasa, Ushna Veerya,and Katu Vipaka, which
help in improving the appetite.
Distention of abdomen was found to be reduced in
28 subjects of study group and 7 subjects in control group after intervention. This can be attributed to
the Vata Anulomana property of Haritaki, which properly digests the Mala and facilitates the passage of Apana Vata.
Pain in abdomen was
reduced in 21 subjects and remained same in 9 subjects of study group and
9 subjects showed reduced symptoms and remained same in 21 subjects in
control group. Shunti and Ajamoda possess Shoolaghna
property, which helped reduced the abdominal pain.
Generalized weakness was reduced in 20 subjects
and remained same in 10 patients. Agnideepaka drugs helped in
normalizing the Agni thereby facilitating digestion and absorption. This
might have helped in reducing the generalized weakness. Reduction in
generalized weakness is also attributed to Yashtimadhu, which is a Jeevaniya
dravya having Balya, Glanihara, and Kshayahara properties.
Headache was reduced in 11 subjects, but remained the same in 19 subjects in
Group A. Body ache was reduced in 13 subjects and remained same in 17 subjects.
Muscle cramp was reduced in 8 subjects and remained same in 22 subjects.
Consistency of stool was improved in 28 subjects
and remained same only in 2 subjects and 8 subjects improved and 22 subjects
remained in control group. Haritaki is Anulomana dravya, which does the Malapaka
resulting in improved consistency of stool.
Frequency of stool was improved in 20 subjects
and remained same in 10 subjects and 3 subjects showed improvement and 27
subjects remain in control group. Sonamukhi is Adhoshodhaka (laxative)
dravya and Saindhava Lavana is Vibandha Hara dravya. Both helped
in improving the stool frequency.
Nature of evacuation was improved in 27 subjects
and 7 subjects in study and control group, respectively. Feeling after
defecation was improved in 29 subjects and 9 subjects in study group and
control, respectively. This was due to the improvements observed in appetite,
digestion, consistency, and frequency of stool. Ingredients of tablet Anuloma
DS were not only effective in facilitating defecation, but also helped in
increasing appetite and digestion. This helped in proper absorption, formation
and elimination of stools. This was significantly evident in secondary outcome
measures such as Constipation Assessment Scale, Patient Assessment Scale of
constipation and Quality of Life Scale.
Functional constipation refers to a condition
where individuals experience hard, infrequent bowel movements that are often
difficult or painful to pass. It is not caused by any apparent physical
abnormalities or specific diseases; instead, it is diagnosed by ruling out
other potential causes.
The current study as demonstrated significant
improvement in signs and symptom of constipation such as stool consistency and
frequency, nature of evacuation, feeling of defecation, reduced appetite, pain
and distention of abdomen, general weakness, headache, body ache, and muscle
cramps with Anuloma DS tablets compared to the lactitol + ispaghula powder in
patients with functional constipation. The improvement observed in PAC-QOL,
Constipation Assessment Scale, Patient Assessment Scale show that Anuloma DS was
highly effective for the treatment in functional constipation vis-à-vis
lactitol + ispaghula powder. It was also safe as no treatment-related
adverse effects were reported by any of the study participants. This beneficial
effect can be attributed to the synergistic therapeutic action of its
constituent herbs.
Ethics Approval
The study was undertaken
after approval by the Institutional Ethics Committee.
1.
Murthy Shrikantha KR (editor). Sushruta Samhita of Vol. III. Reprint ed. (India, Varanasi: Chaukhambha Orientalia), Uttara Tantra 2017, 55/7.
2.
Rajput M, Saini SK. Prevalence of constipation among the general population: a community-based survey from India. Gastroenterol Nurs. 2014;37(6):425-9.
3.
Forootan M, Bagheri N, Darvishi M. Chronic constipation: a review of literature. Medicine (Baltimore). 2018;97(20):e10631.
4.
Wald A, Scarpignato C, Mueller-Lissner S, Kamm MA, Hinkel U, Helfrich I, et al. A multinational survey of prevalence and patterns of laxative use among adults with self-defined constipation. Aliment Pharmacol Ther. 2008;28(7):917-30.
5. Varuni BG. An open-labeled clinical
study to evaluate the safety and efficacy of “Anuloma DS” in improving constipation. Indian J Clin Pract. 2023;34(2):15-22.
6.
Lacy BE, Patel NK. Rome criteria and a diagnostic approach to irritable bowel syndrome. J Clin Med. 2017;6(11):99.
7.
Jani B, Marsicano E. Constipation: evaluation and management. Mo Med. 2018;115(3):236-40.
8.
Chatoor D, Emmnauel A. Constipation and evacuation disorders. Best Pract Res Clin Gastroenterol. 2009;23(4):517-30.
9.
Locke GR 3rd, Pemberton JH, Phillips SF. American Gastroenterological Association Medical Position Statement: guidelines on constipation. Gastroenterology. 2000;119(6):1761-6.
10.
Portalatin M, Winstead N. Medical management of constipation. Clin Colon Rectal Surg. 2012;25(1):12-9.